Collagenase clostridium histolyticum
1 College of Human Medicine, Michigan State University, Marquette General Healthcare/Duke LifePoint, Marquette, USA
Introduction
Collagenase clostridium histolyticum (CCH); XIAFLEX®) is approved for use in the US (as Xiaflex®) and Europe (as Xiapex®) for the treatment of Dupuytren’s contracture with a palpable cord in adult patients [1] [2]. This agent is the only commercially available injectable CCH for Dupuytren’s treatment [3]. CCH is a mixture of 2 microbial collagenases, Collagenase AUX-I and Collagenase AUX-II, which are isolated and purified from the fermentation of Clostridium histolyticum bacteria. Collagenase AUX-I is a single polypeptide chain consisting of ~1,000 amino acids of known sequence. This collagenase has an observed molecular weight of 114 kiloDaltons (kDa) and belongs to the Class I Clostridium histolyticum collagenases [1]. Collagenase AUX-II is a single polypeptide chain consisting of ~1,000 amino acids of deduced sequence. It has an observed molecular weight of 113 kDa and belongs to the Class II Clostridium histolyticum collagenases [1].
CCH dosing, pharmacokinetics, and pharmacodynamics
Dosing overview
The dose of CCH is 0.58 mg injected into a palpable cord to treat contracture of a metacarpophalangeal (MP) or a proximal interphalangeal (PIP) joint [1]. Approximately 24 hours after injection, a finger extension procedure is performed (with local anesthetic injection) to effect cord disruption if the contracture persists. If an MP or PIP contracture remains 4 weeks after CCH injection and finger extension, the cord may be re-injected with another dose of 0.58 mg of CCH and the finger extension procedure repeated (at ~24 hours post-injection). Injections and finger extension procedures may be repeated up to a total of 3 times per cord at ~4-week intervals, if needed. Only 1 cord is treated at a time; cords may be injected with CCH in a sequential order if a patient has multiple palpable cords producing MP and/or PIP contractures.
Pharmacokinetics
Following administration of a single CCH dose of 0.58 mg into a Dupuytren’s cord in 20 patients, no quantifiable levels of CCH (AUX-I or AUX-II) were detected in plasma up to 30 days post-injection [1]. Direct elimination and tissue distribution studies could not be conducted because detectable levels of CCH could not be confirmed [3]. Since no significant systemic exposure was seen in human subjects after injection, collagenase appears to remain relatively confined to the local tissues after injection [3]. CCH functions in its native form and does not require proteolytic cleavage to be activated [3]. It is not a substrate for drug metabolizing pathways such as cytochrome P450. In vitro studies have shown that most collagen digestion was completed by 24 hours after exposure to collagenase [4].
Pharmacodynamics
CCH causes lysis and breakdown of the 3-dimensional structure of its collagen substrate (Figure 1) [3].
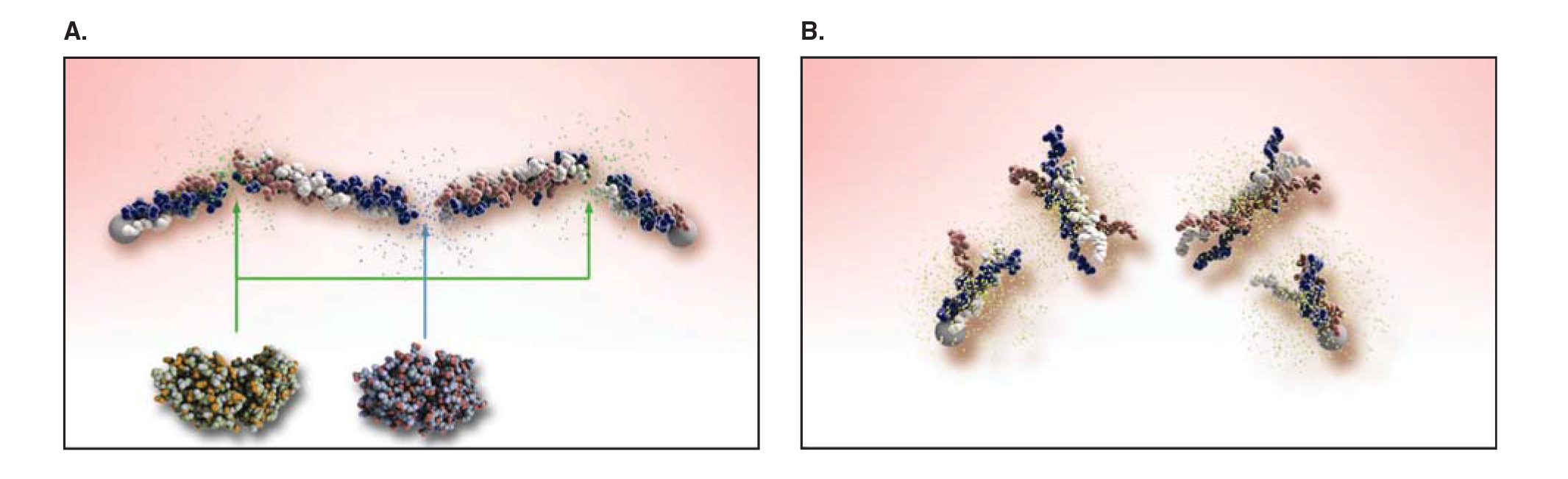
Each enzyme molecule requires active catalytic and collagen-binding domains in order to possess catalytic activity against collagen [3]. The enzymes require both calcium and zinc to act as metal cofactors to facilitate the lytic process [3]. Zinc is necessary for activation at the catalytic site, and calcium maintains the appropriate structure of the collagen binding site to accept the triple-helix structure of the collagen fibrils. When collagenase is injected directly into Dupuytren’s cords, it specifically targets the collagen within the diseased cord, which has an abundant amount of type I and III collagen [3]. These enzymes lyse the cord’s collagen structure to make it more susceptible to rupture [3].
Importantly, both classes of collagenase are not immunologically cross-reactive and have broad catalytic effects on all collagen types, except for type IV collagen, which is found in the basement membranes of blood vessels and the perineurium of peripheral nerves [3]. In addition, nonclinical studies, including animal models, did not demonstrate significant degradation of blood vessels, nerves, and epithelium following local injection, and this may be related to its poor activity against type IV collagen [3], [5], [6].
Mechanism of action
Overview
Collagenases are proteinases that hydrolyze collagen in its native triple-helical conformation under physiological conditions, resulting in lysis of collagen deposits [1] and, when injected into a Dupuytren’s cord, in the enzymatic disruption of that cord [1].
Biomedical and structural aspects of CCH
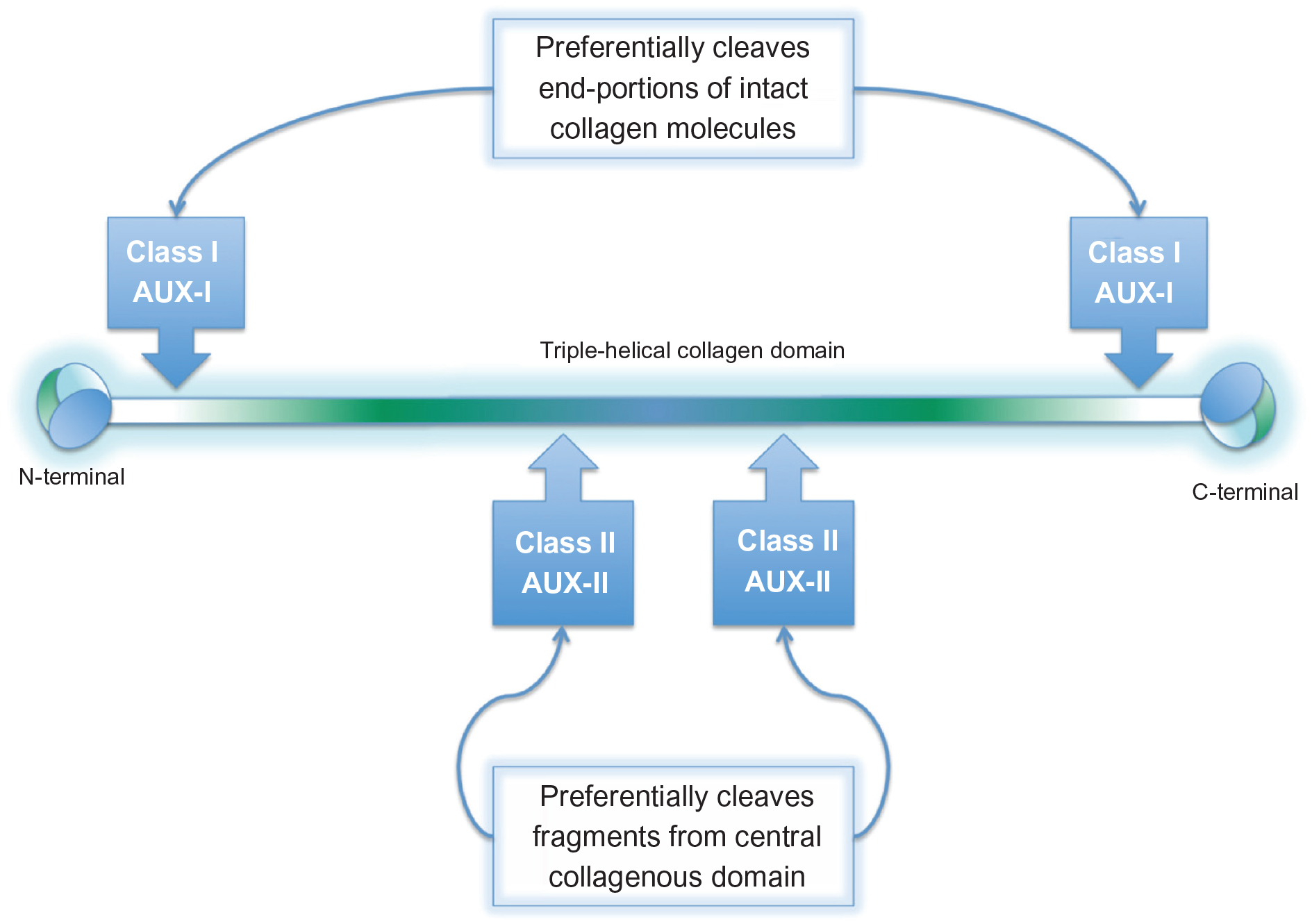
Collagenases are categorized into 1 of 2 classes based on gene of origin, protein domain, and substrate specificity [3]. AUX-I and AUX-II have been shown by substrate activity patterns to be representative of the Class I (ColG) and Class II (ColH) collagenases, respectively, and differ in preferred cleavage site on the collagen molecule. Class I enzymes act at loci near the ends of the collagen triple-helical domains, whereas Class II enzymes cause internal cleavages (Figure 2) [4], [7]. Pre-clinical studies demonstrate that Class I and Class II collagenases work synergistically and are more effective together than if acting independently [3].
Collagen degradation
The molecular mechanism of collagen lysis involves a 2-state model of bacterial collagen lysis, where recognition and unraveling of collagen microfibrils into triple helices and unwinding of triple helices are driven by collagenase opening and closing [8]. Figure 3 is a 6-step description of the unified processing model of triple-helical and microfibrillar collagen lysis [8].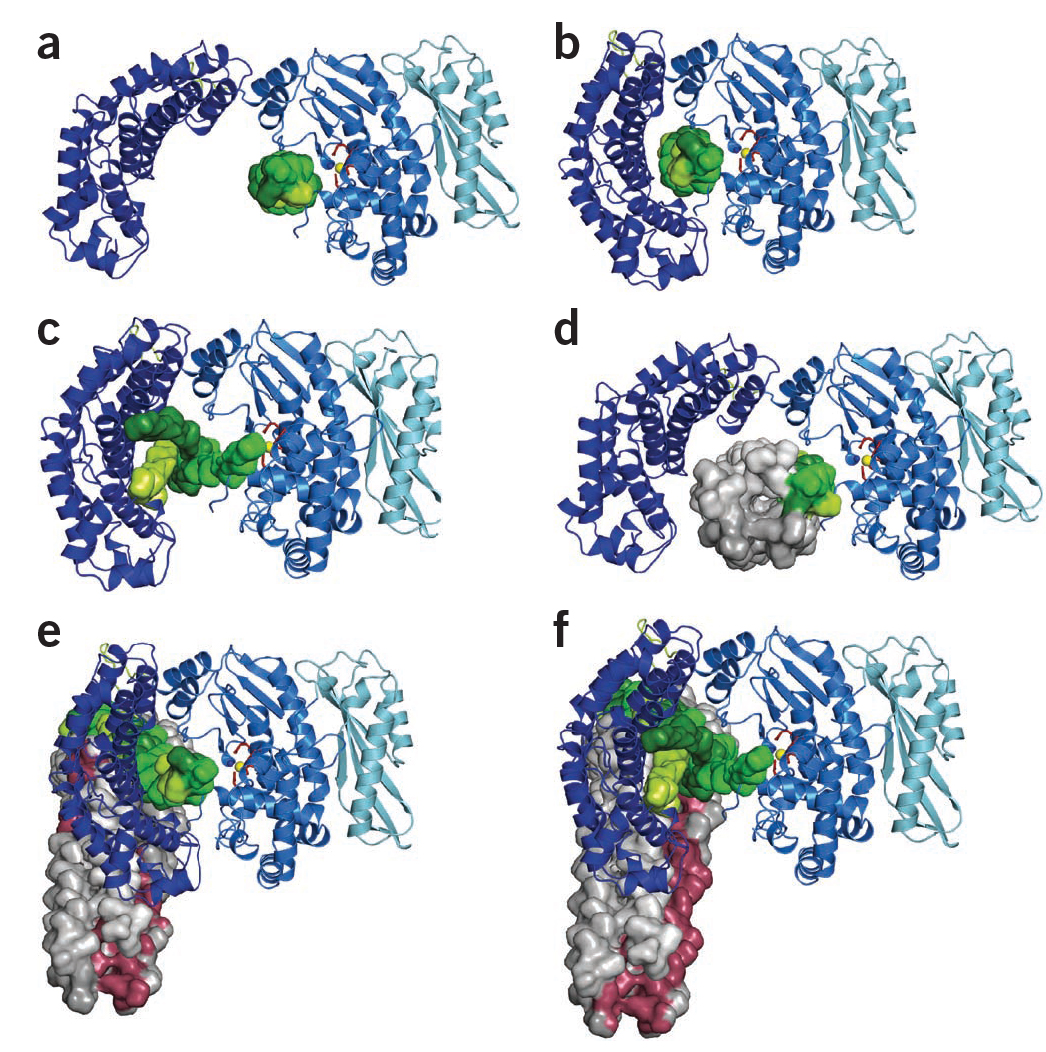
Synergistic activity
Pre-clinical studies demonstrated that the combination of Class I and Class II collagenases working synergistically is more effective in collagen digestion than either acting alone or simple addition of the two [3]. In a study by Kono, which characterized collagenolytic enzymes from Clostridium histolyticum, the combination of Collagenase I and II denatured collagen more rapidly than either individually (Figure 4) [9].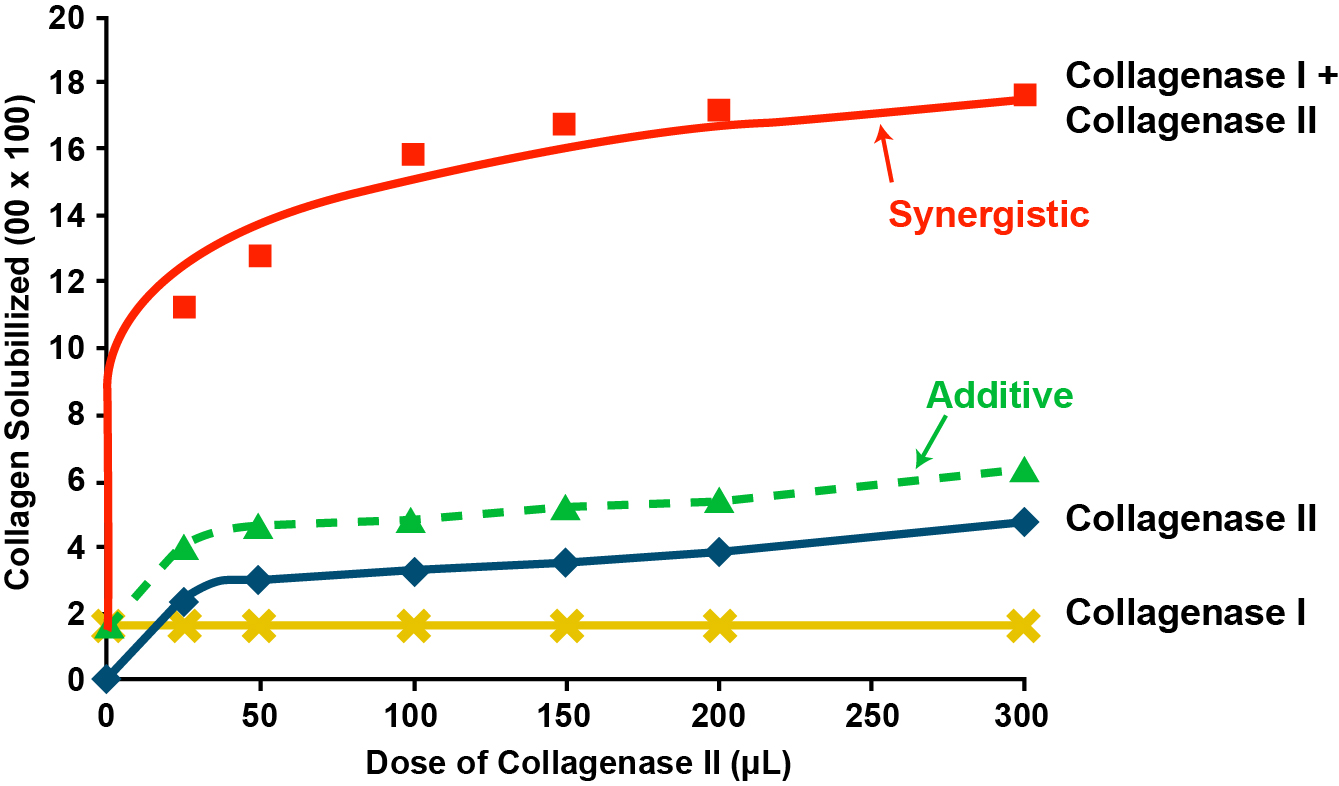
In vitro/In vivo collagen degradation
CCH has been demonstrated to elicit a well-circumscribed focal degradation of collagen. The potential adverse extravasation of CCH from an injection site to adjacent collagen-containing structures was assessed in a rat tail tendon model, which resembles the structure of a human finger [10]. At 150 and 300 collagenase units, there was no detectable adverse extravasation to adjacent tissues, including muscle, nerve, other tendons, vessels, bone, and skin [10]. Due to the highly potent binding affinity in their native (in vivo) conformation, the enzymes’ primary in vivo activity is to selectively degrade the relevant pathologic collagen subtypes (types I and III) that constitute Dupuytren’s cords [4].
Clostridial collagenase is not effective at degrading type IV collagen in vivo despite the ability of the collagen binding domain from Class I collagenase to recognize type IV collagen (which is the primary component of vascular basement membranes and the perineurium) [4]. Purified clostridial collagenase had no significant activity against type IV collagen in a synthetic basement membrane model [4]. Importantly, no degradation of blood vessel basement membranes was detected following subcutaneous injection in rats, nor were any effects on blood vessels, nerves, and epithelium noted following local injection in the nonclinical studies [4].
Clinical trial overview
A total of 13 (one phase 1, three phase 2, and nine phase 3) clinical studies were conducted in patients with Dupuytren’s contracture in the US, Europe, and Australia. Eligible patients had a diagnosis of “advanced Dupuytren’s Disease,” with a fixed-flexion deformity (i.e., ≥20º but ≤80º for PIP joints; ≥20º but ≤100º for MP joints) of ≥1 finger other than the thumb caused by a palpable cord, and with a positive “table top test” defined as the inability to simultaneously place the affected finger(s) and palm flat on a table [11]. Overall, a total of 1,082 subjects received ≥1 injection of CCH 0.58 mg in these studies [4].
Phase 2 trials
Phase 2 open-label, dose-escalation trial
In a phase 2 open-label, dose-escalation trial, 35 patients with Dupuytren’s Disease were enrolled (32 men, mean age of 65 years) [12]. The initial 6 patients were treated using a dose-escalation protocol, where 300, 600, 1,200, 2,400, 4,800, and 9,600 units (U) of collagenase were injected into the cord causing an MP joint contracture; however, no beneficial clinical effects were observed [12]. The remaining 29 patients received a 10,000 U collagenase injection for contractures of 34 MP joints, 9 PIP joints, and 1 thumb. In 28/34 (82.4%) of patients, the MP joint contractures corrected to 0°; 2/34 (6.0%) corrected to 5°; with full range of motion (ROM) within 14 days [12], a success rate of 88%. For the PIP joint contractures, 4/9 (44.4%) corrected to 0°; in addition, 1 PIP joint corrected to 10° and 2 to 15°. Eight patients had multiple corrections, with 4 having MP/PIP correction of the same finger and 4 having MP/MP correction of adjacent fingers [12]. This pilot dose-escalation study determined that 10,000 U collagenase was the clinically safe and effective dose for inducing cord rupture in both MP and PIP joints [12].
Phase 2 randomized, placebo-controlled, single-dose study
In a phase 2 randomized, double-blind, placebo-controlled study of CCH injection, 36 patients with MP joint contractures (31 men, mean age of 65 years; contractures included 20 small fingers, 13 ring fingers, 2 middle fingers, and 1 thumb) and 13 patients with PIP joint contractures only (11 men, mean age of 64.3 years; contractures were in 5 ring and 8 small fingers) received a single dose of 10,000 U versus placebo (1:1 ratio) [13]. Time to return to normal extension was significantly less for the patients with MP joint contractures receiving CCH (P=0.001). In the 10,000 U collagenase treatment group (n=18), half of patients showed a reduction in contracture to within 0° to 5° by 7 days after injection, compared with only 2/18 patients receiving placebo [13]. One month after injection, 14/18 patients in the collagenase treatment group showed correction to 0° to 5°, compared with 2/18 patients who received placebo. There were 4 recurrences of MP joint contracture during the subsequent 4-year follow-up [13]. For patients with PIP contractures, 5/7 patients corrected to 0° to 5° one month from 1 injection; 1 corrected to normal extension after a second 10,000 U injection 1 month later; and there was 1 failure. Six of 6 patients who received placebo did not correct. Upon secondary treatment with collagenase, 4/6 corrected to 0° after 1 month. There was a failure to achieve clinical success in 1 patient, and 1 patient was lost to follow-up evaluation. There were 4 recurrences of PIP joint contracture during the next 3.8 years. Adverse effects were local and minimal, and included pain when the cord ruptured, pain to pressure at the injection site, dorsal and volar hand edema, minimal hematoma, and limited ecchymosis involving the treated hand. In approximately a third of patients (especially those who received PIP injections), elbow and/or axillary lymphadenopathy was noted. All effects resolved within 14 days of injection [13].
Phase 2 randomized, placebo-controlled, dose-response study
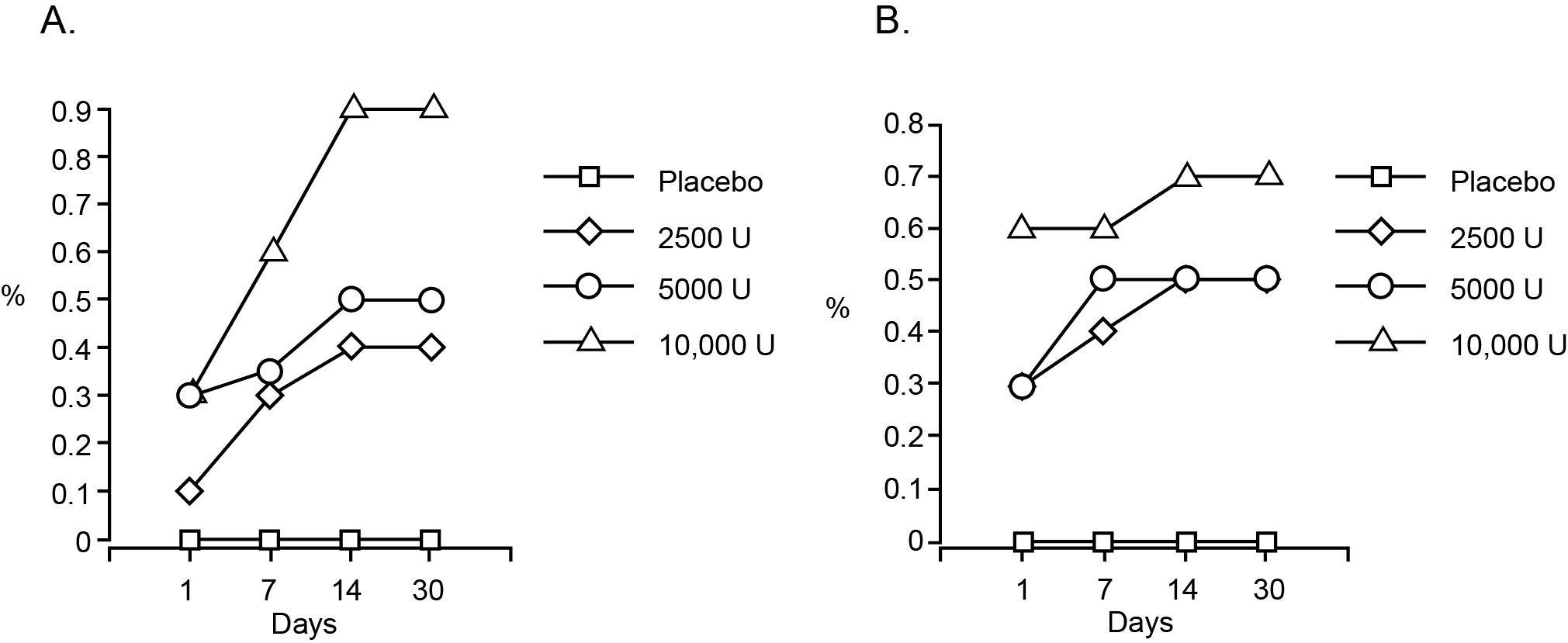
Because the results of the phase 2 single-dose trial described in the previous paragraph clearly demonstrated that 10,000 U collagenase injection corrected patients’ contractures, a phase 2, randomized, placebo-controlled, double-blind, dose-response study of collagenase injection was undertaken to determine whether 10,000 U was the minimum safe and effective dose in a larger number of patients [13]. Eighty patients (64 men, mean age of 63.9 years) were enrolled; 55 had MP contractures and 25 had PIP contractures of 50 small fingers, 23 ring fingers, and 7 middle fingers. Patients were randomized to receive 2500 U (n=18), 5000 U (n=22), or 10,000 U (n=23) of CCH or placebo (n=17) [13]. Comparison of dose groups showed that the “success” rate (correction to 0°–5°) was significantly higher in patients treated with 10,000 U of collagenase at 1 month (P=0.0002), with 18/23 having full extension by 1 month, compared with 10/22 and 9/18 patients receiving 5000 and 2500, respectively. There was no response to placebo injection in any patient. Figure 5 shows the success rate (hazard function) for each treatment group for the MP joints; by Day 14 after 10,000 U injection there was a 90% success rate. A log rank test was performed for evaluation of treatment differences and was significant at P=0.0002. The overall clinical success for PIP joint patients was significant at a 10,000 U dose with a 70% success rate (P=0.0397) and demonstrated the recovery of extension in the PIP joint using CCH [13].
Phase 3 clinical trials
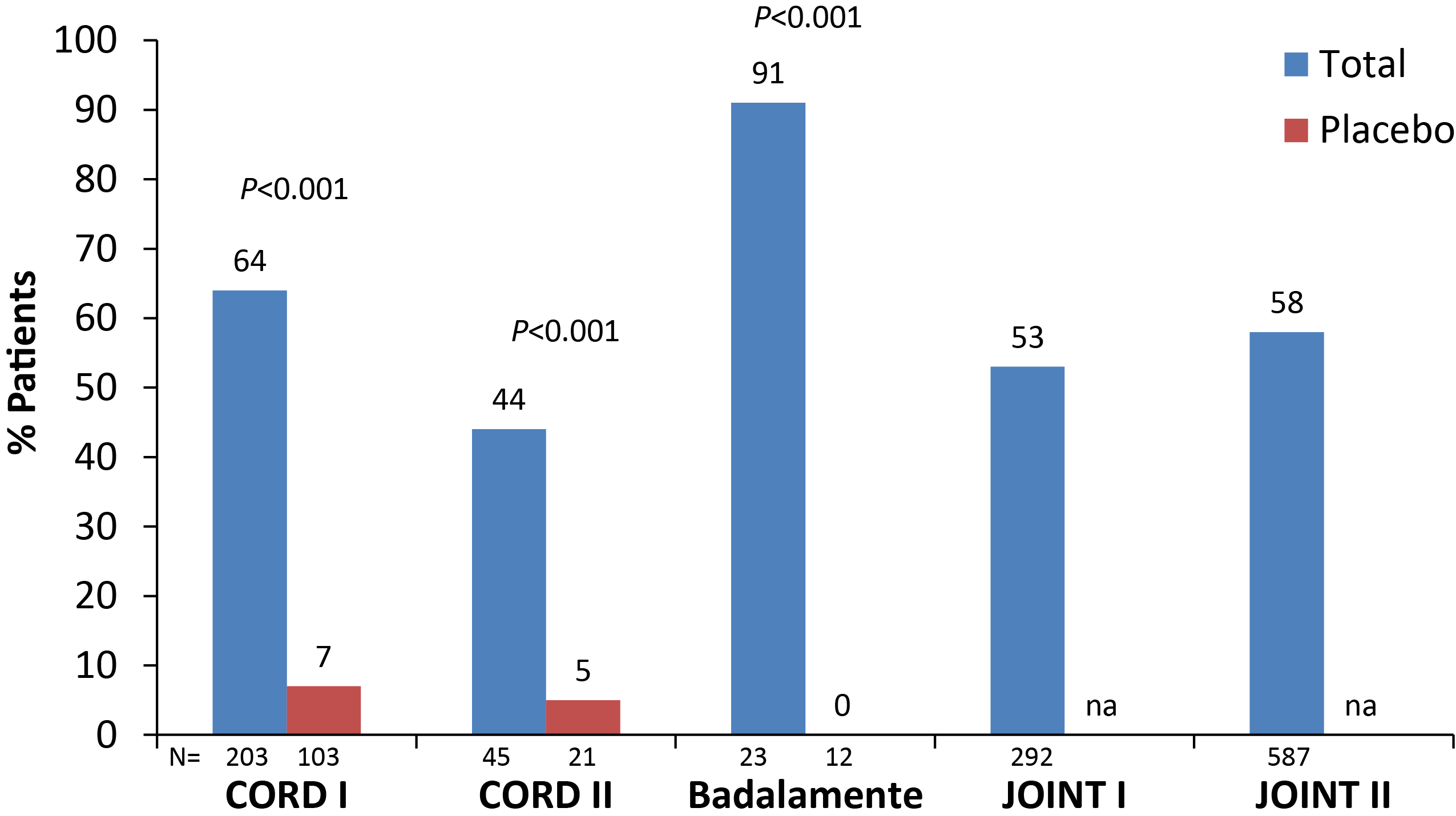
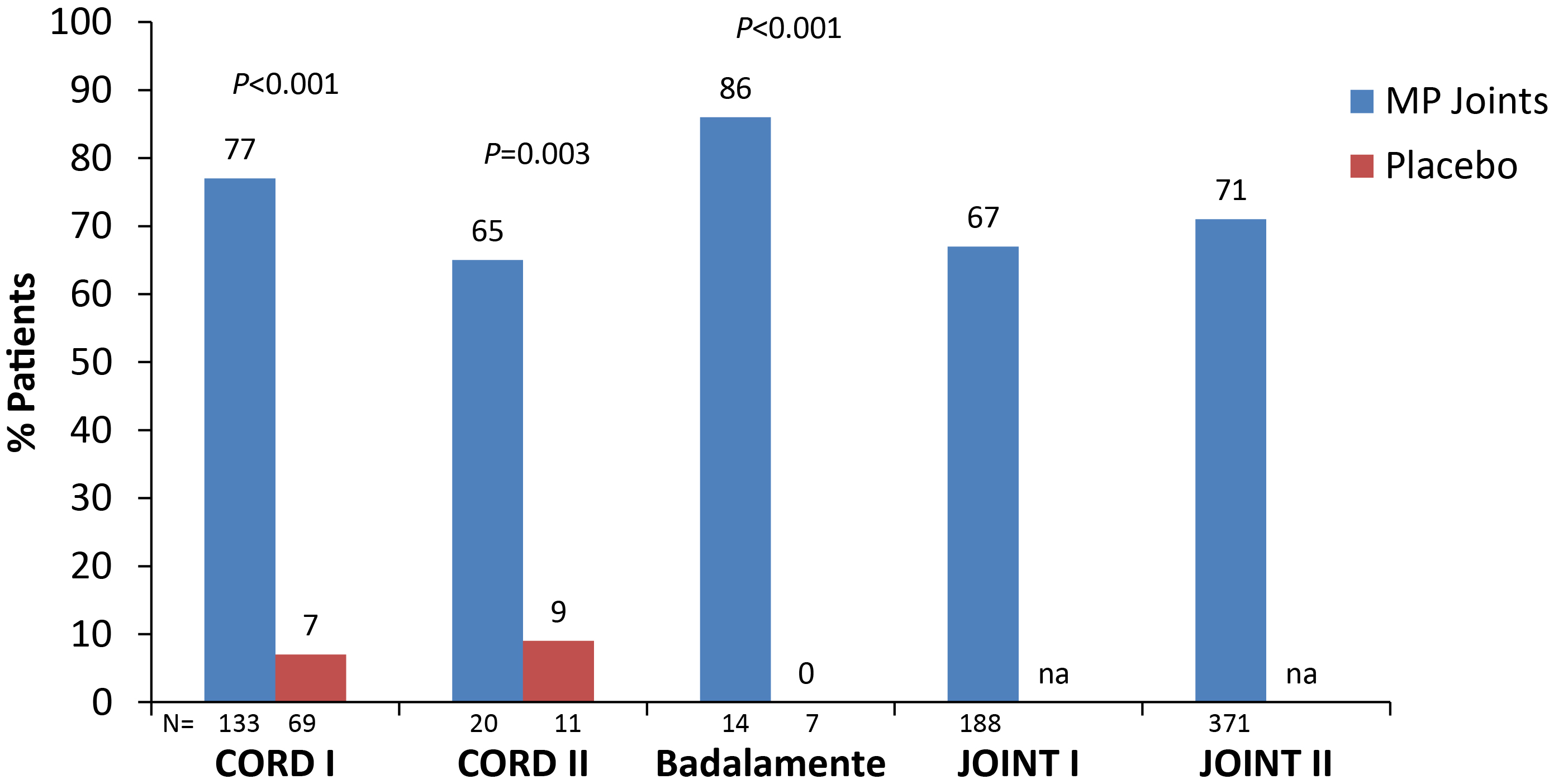
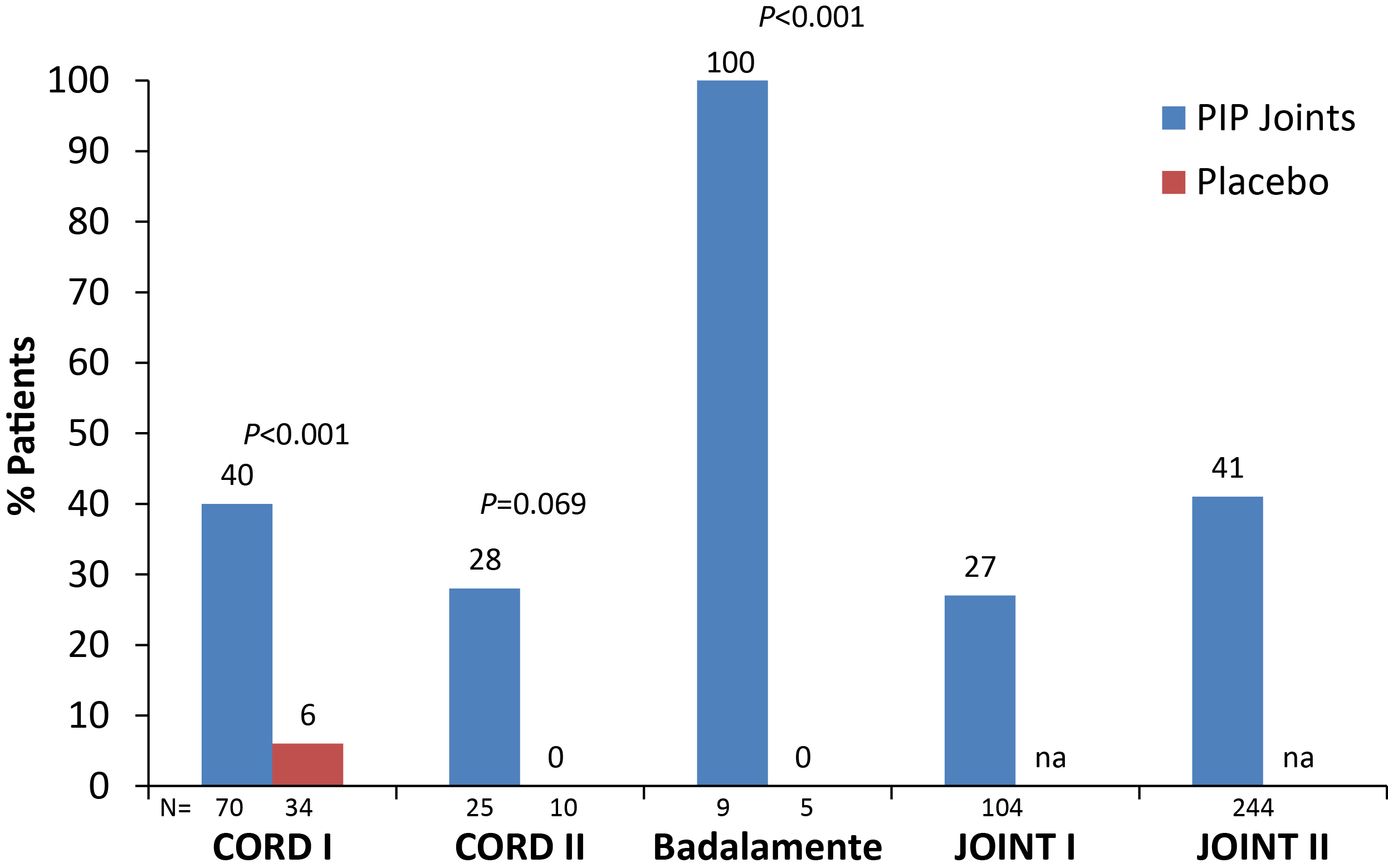
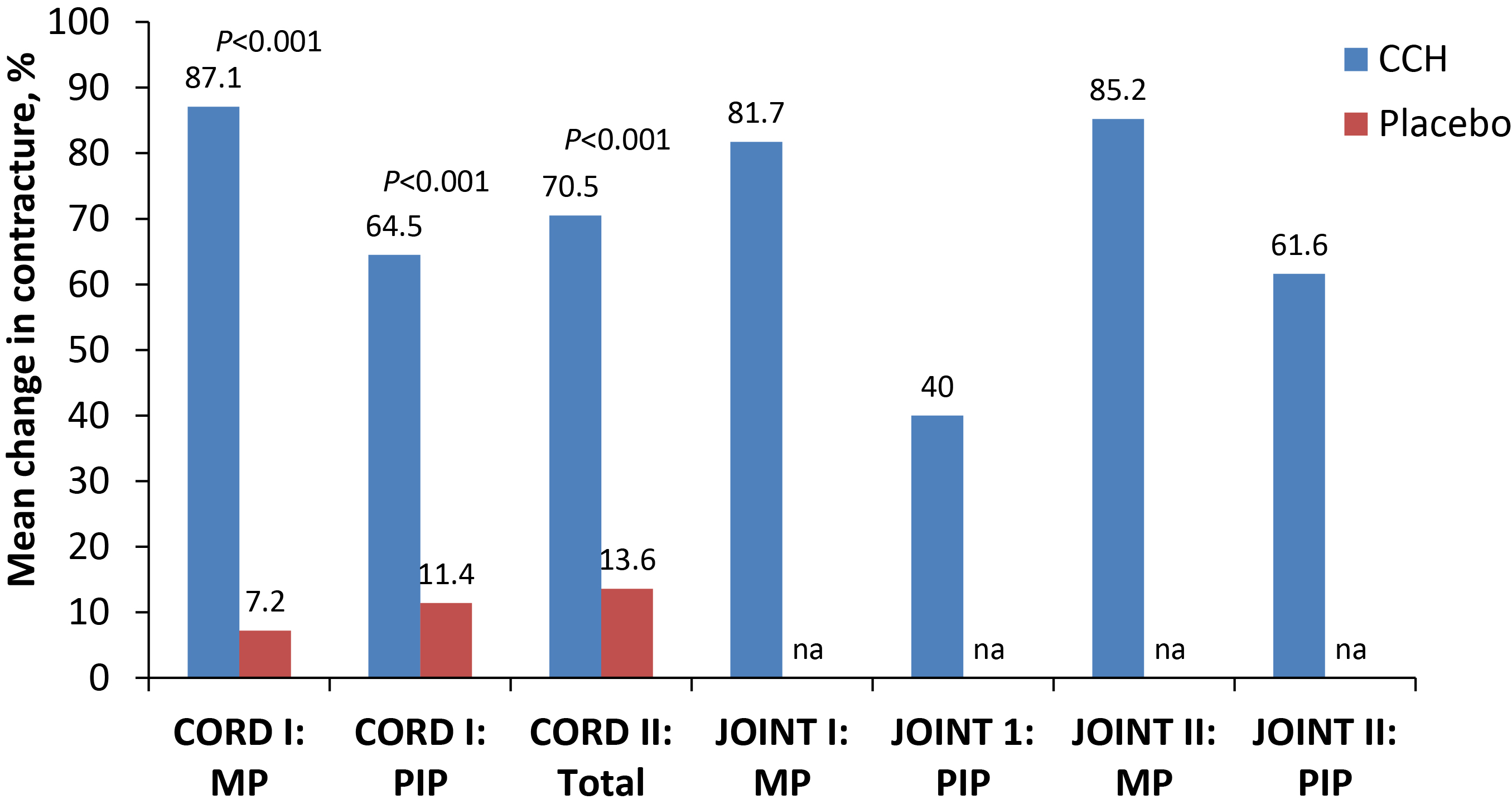
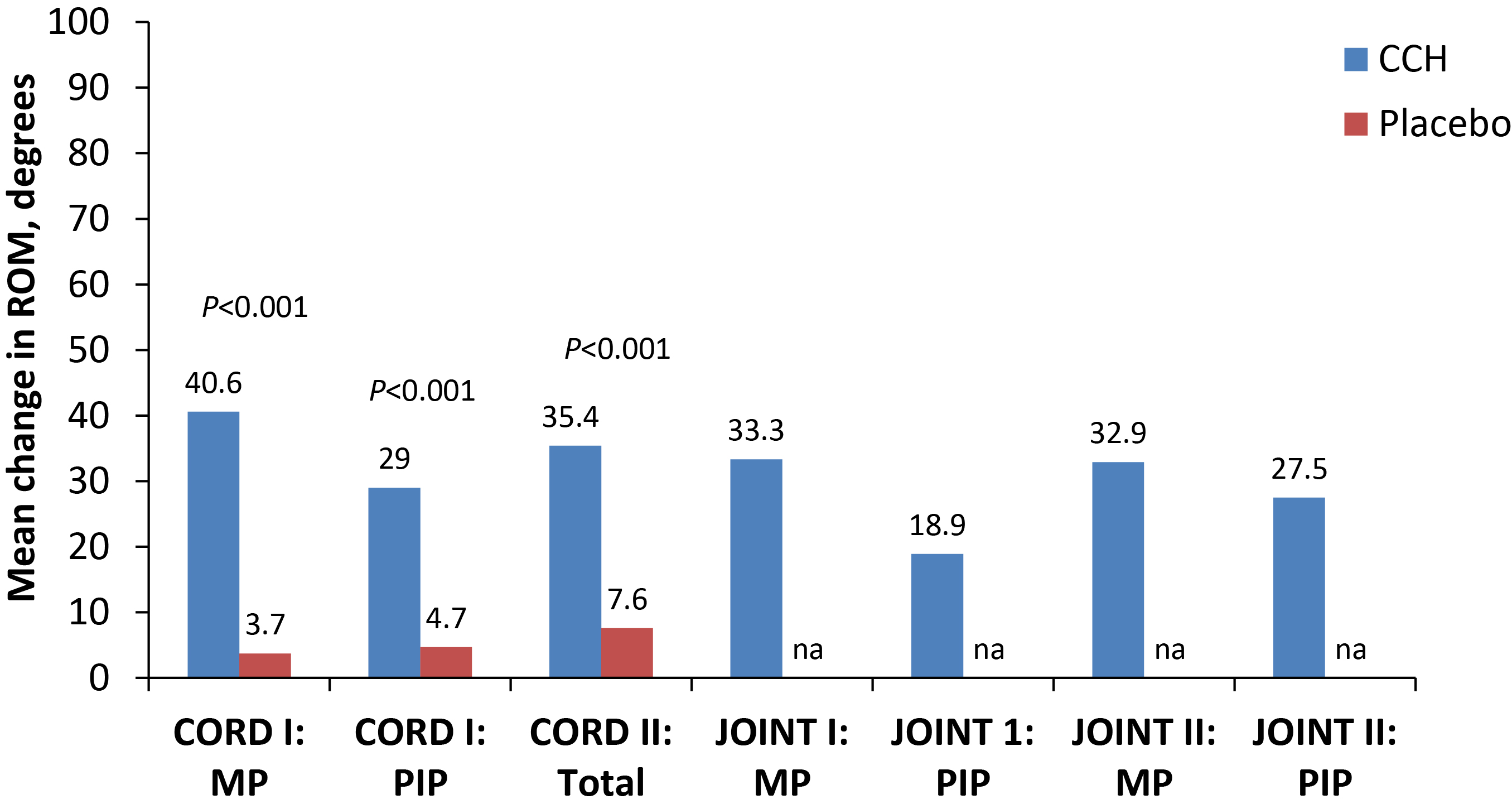
The major phase 3 studies consisted of randomized, placebo-controlled clinical trials, CORD I, CORD II, and a study by Badalamente et al, as well as 2 open-label trials, JOINT I and JOINT II [14], [15], [16], [17].
Trial designs
The Collagenase Option for the Reduction of Dupuytren’s (CORD I US and CORD II AU) studies were prospective, multicenter, phase 3 clinical trials comprising 90-day, randomized, double-blind, placebo-controlled phases and ongoing open-label extensions (Figure 6) [14], [15].
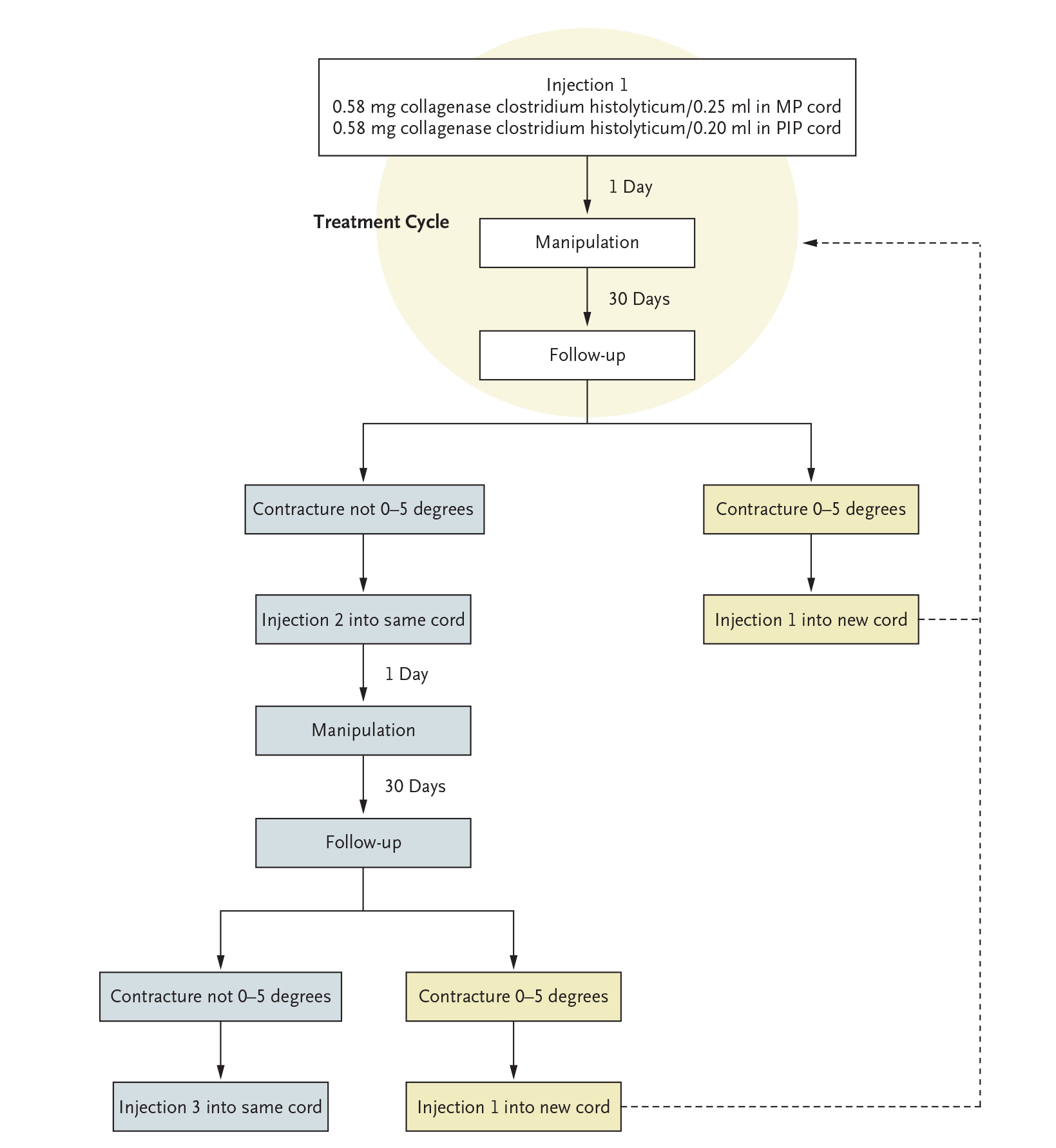
Badalamente et al. (2007) conducted a phase 3, randomized, double-blind, placebo-controlled trial followed by an open-label extension of ≤12 months after last injection [17]. JOINT I and II were concurrent 9-month, open-label studies which evaluated the efficacy and safety of CCH (0.58 mg) to reduce the degree of contracture in patients with advanced Dupuytren’s contracture [16].
Patient populations
CORD I and II, the Badalamente et al. (2007) study, and JOINT I and II: Adult patients with Dupuytren’s Disease who had MP joint contractures ≥20° and ≤100° or PIP contractures of 20° to 80° and were unable to simultaneously place the affected finger and palm flat on a table. For all phase 3 trials, investigators identified a “primary joint” for treatment in each patient [14], [15], [16], [17], [18].
Secondary and tertiary joints were also identified for possible subsequent injections [14], [15], [16], -[17]. CCH (0.58 mg per injection) or placebo was reconstituted in 0.25 mL of sterile diluent for MP joints or 0.20 mL of sterile diluent for PIP joints [14], [15], [16] and was injected into the affected cords [14], [15], [16], [17]. Follow-up visits occurred 1, 7, possibly 14, and 30 days after injection [14], [15]. In the JOINT I and II open-label trials, patients received up to five 0.58 mg CCH injections prepared in the same manner as in the CORD trials. There were 5 treatment cycles, with a maximum of 3 injections per cord, separated by ≥30 days; only 1 cord could be injected within a given treatment cycle [16].
Treatment cycles
In CORD I and CORD II, a treatment cycle comprised injection, manipulation, and 30-day follow-up [15], [18]. In CORD I, each affected cord that was contracting the joint could undergo a maximum of 3 treatment cycles, and each patient could receive a maximum of 3 injections during the double-blind phase [14]. In CORD II, each patient could receive a maximum of 8 treatment cycles during the 12-month study [15]. In JOINT I and II, a treatment cycle consisted of 1 CCH injection for MP joints and PIP joints, followed by a series of evaluations [16].
Outcome measures
For all phase 3 trials, the primary endpoint was contracture correction to 0° to 5° by 30 days post-injection. Recurrence of contracture post-treatment was defined as an increase in joint contracture of ≥20° in the presence of a palpable cord [14], [15], [16], [17].
- Additional/secondary endpoints included the following: In CORD I, recurrence of contracture, defined as a decrease in joint contracture to 20° or more in the presence of a palpable cord at any time during the study [14].
- In JOINT I/II, secondary end points included clinical success at 30 days, percentage of joints achieving ≥50% reduction from baseline contracture (defined as having achieved clinical improvement), percentage of decrease in degree of joint contracture from baseline to after the last CCH injection, and increase in ROM (in degrees) between full-flexion and full-extension angles [16].
- In the study by Badalamente et al, additional efficacy variables included: time required to achieve success (correction to 0°–5° of normal) in the primary joint in the double-blind phase, the number of injections required to achieve success, and recurrence, defined as a return of contracture (≥20°) in successfully treated joints [17].
Efficacy results
Primary and other efficacy outcomes for the phase 3 trials (MP and PIP joints) are in Figures 7a to 7c and Figures 8 and 9 [14], [15], [16], [17].
Phase 3 results: patient satisfaction
After collagenase treatment (i.e., day 30), patients who rated themselves as ‘very satisfied’ or ‘quite satisfied’ were in the ‘normal’ category of severity for ROM (80.8° and 71.9°, respectively); patients who were ‘neither satisfied nor dissatisfied’ were in the ‘mild’ category (63.0°); and patients who were ‘quite dissatisfied’ or ‘very dissatisfied’ were in the ‘moderate’ category (54.2° or 45.3°, respectively). In the collagenase group, 87% of patients reported being ‘very satisfied’ or ‘quite satisfied’ with treatment compared with 32% in the placebo group (P<0.001). Greater treatment satisfaction was correlated with improved ROM (R=0.51; P<0.001) [19]. In JOINT I and JOINT II, 71% of patients were ‘very satisfied’ and 21% ‘quite satisfied’ with treatment [16].
CCH: Safety and tolerability
Adverse events (AEs)
In the placebo-controlled portions of CORD I and CORD II, through day 90, 98% and 51% of CCH- and placebo-treated patients, respectively, had an AE after up to 3 injections. Over 95% of XIAFLEX-treated patients had an adverse reaction of the injected extremity after up to 3 injections; ~81% of these local reactions resolved without intervention within 4 weeks of CCH injections [1]. Treatment-emergent adverse events (TEAEs) occurring in ≥5% of patients in both CORD and both JOINT trials are listed below (Table 1). Overall, patients who received CCH had significantly more injection- and manipulation-related events (e.g., contusion, injection-site hemorrhage, injection-site pain, pain in the upper extremity, tenderness, ecchymosis, injection-site swelling, pruritus, skin laceration, lymph node enlargement and tenderness on palpation, lymphadenopathy, erythema, blister, injection-site pruritus, and axillary pain) than those who received placebo injections (P≤0.02) [14]. Most treatment-related AEs were mild to moderate in intensity and resolved ≤14 days without intervention [14], [15], [16].
| CORD I | CORD IIa | Joint I/II | |||
|---|---|---|---|---|---|
| CCH* | PBO | CCH | PBO | CCH | |
| (n=204) | (n=104) | (n=45) | (n=21) | (n=587) | |
| Injection Site Reactions | |||||
|
76 (37.3) | 4 (3.8) | 19 (42.2) | 0** | 216 (37) |
|
66 (32.4) | 5 (4.8) | 17 (37.8) | 2 (9.5)** | 248 (42) |
|
43 (21.1) | 4 (3.8) | 16 (35.6) | 3 (14.3) | 156 (27) |
|
11 (5.4) | 0 | NR | NR | NR |
|
NR | NR | 2 (4.4) | 0 | 34 (6) |
| Edema, peripheral or other | 148 (72.5) | 4 (3.8) | 35 (77.8) | 2 (9.5)** | 439 (75) |
| Contusion | 104 (51.0) | 2 (1.9) | 33 (73.3) | 2 (9.5)** | 350 (60) |
| Upper-extremity pain | 63 (30.9) | 3 (2.9) | 22 (48.9) | 2 (9.5)** | 224 (38) |
| Tenderness | 54 (26.5) | 0 | 6 (13.3) | 0 | 146 (25) |
| Ecchymosis | 51 (25.0) | 1 (1.0) | NR | NR | 41 (7) |
| Pruritus | 22 (10.8) | 1 (1.0) | 5 (11.1) | 0 | 59 (10) |
| Skin laceration | 22 (10.8) | 0 | NR | NR | 55 (9) |
| Lymph-node enlargement | 21 (10.3) | 0 | NR | NR | NR |
| Lymphadenopathy | 20 (9.8) | 0 | 11 (24.4) | 0** | 42 (7) |
| Erythema | 13 (6.4) | 0 | NR | NR | NR |
| Blister | 11 (5.4) | 0 | NR | NR | 48 (8) |
| Axillary pain | NR | NR | 5 (11.1) | 0 | 45 (8) |
| Hematoma | NR | NR | NR | NR | 45 (8) |
|
*P≤0.02 compared with placebo; **P≤0.05 compared with placebo; NR=not reported. |
|||||
Serious AEs
In CORD I, 7 patients who received collagenase had an SAE. Three of the 7 were deemed to be treatment related: 1 case of complex regional pain syndrome and 2 flexor tendon ruptures, both of which required surgical procedures; 1 tendon rupture was treated by excision of the ruptured tendon and tenolysis of the remaining tendon, and the other had flexor tendon reconstruction [14]. In CORD II, 1 serious TEAE was reported: a patient had a flexion pulley rupture of the left small finger and subsequently underwent PIP joint arthrodesis and tenotomy [15]. In JOINT I and II combined, 2 patients had serious AEs that were possibly or probably related to study drug (deep vein thrombosis in the leg and tendonitis near the injection site). No tendon ruptures occurred [16].
Flexor tendon rupture
While tendon rupture associated with CCH treatment is rare – of over 300 patients who had over 1,000 injections in the 3 randomized, double-blind, placebo-controlled studies (CORD I, CORD II, and the Badalamente et al study), 2 flexor tendon ruptures were reported out of 444 injections – it is a very serious adverse event of treatment [20]. The reported incidence of tendon rupture was 0.3% in controlled and uncontrolled studies of CCH treatment (n=1,082) [1], [21]. The flexor tendon ruptures occurred when CCH was used to treat PIP flexion contractures of the small finger [20].
Immunogenicity
During clinical studies, patients were tested at multiple time points for antibodies to the protein components of CCH. At 30 days following first injection of CCH 0.58 mg, 92% and 86% of patients had antibodies detected against AUX-I and AUX-II enzymes, respectively. After a fourth injection, every CCH-treated patient demonstrated high titers of antibodies to both AUX-I and AUX-II. Neutralizing antibodies to AUX-I or AUX-II were detected in 10% and 21%, respectively, of patients treated with CCH. However, no correlation of antibody frequency, antibody titers, or neutralizing status to clinical response or to adverse reactions was found [1].
CCH treatment in special patient populations
CCH has been shown to be an effective treatment for Dupuytren’s contracture in a variety of patient populations, including high-risk patients, and those with comorbidities, multiple Dupuytren’s Disease cords, or severe PIP joint contractures [22], [23], [24], [25], [26].
- Increased surgical risk
Pooled data from CORD I, CORD II, and the 2007 Badalamente study showed that there was no significant difference in clinical success by age, diabetes status, or difference in adverse events among the subgroups; with peripheral edema, contusion, and injection site hemorrhage being most common [14], [15], [17], [22]. Raven et al concluded that high-risk subgroups do not demonstrate differences in efficacy or safety with CCH treatment of Dupuytren’s-related contractures [22]. - Multiple cord injections
In an open-label phase 3b study (N=60), Coleman et al assessed the safety and efficacy of two 0.58 mg CCH doses injected into cords in 2 joints of the same hand during the first visit, followed by finger extension ~24 hours later [24]. Mean total (sum of the 2 joints treated) flexion contracture decreased from 87° to 24° (76%; MP: 86%; PIP: 66%) [24]. Mean total ROM increased from 100° to 161°, and clinical success was achieved in 76% and 33% of MP and PIP joints, respectively [24]. They concluded that 2 cords can be treated concurrently while maintaining efficacy and safety of cords treated individually and sequentially [24]. Multiple concurrent injections would eliminate the 30-day wait between single treatments and allow for more rapid treatment of patients with multiple affected joints. - Severe PIP deformity
Skirven et al assessed the effects of a specific orthotic intervention and therapy protocol on PIP joint contractures >40° for 22 fingers in 21 patients (mean age of 63 years [37–80 years]) [26]. Following CCH treatment, the contracture significantly decreased to a mean of 12° (range, 0°–36°) 1 week after cord rupture and therapy (P<0.002). By 4 weeks, the mean contracture was 7° (range, 0°–35°) (P<0.002). The differences in PIP joint contracture were statistically significant and represented 88% improvement. - Previous hand surgery
Bainbridge et al assessed the efficacy and safety of CCH in patients with previous Dupuytren’s contracture surgery by pooling data from 12 CCH clinical trials [25]. Of 1082 patients screened, 422 (39%) had previous surgery [25]. After treatment with CCH, fixed flexion contracture (FFC) at MP joints was reduced by 75% in previously operated hands and by 80% for non-operated hands (P=0.6). Improvements in ROM were 32° and 32°, respectively (P=0.9). For PIP joints, the reductions in FFC for the operated and non-operated hands were 52% and 50%, respectively (P=0.6); improvements in ROM were 24° and 26°, respectively (P=0.3).
Long-term efficacy and safety/tolerability: CCH treatment
Cordless study: 3-year interim data
The interim cumulative 3-year recurrence in CCH-treated joints achieving the primary efficacy endpoint (i.e., FFC ≤5° in the index study) is reported here, as is the durability of response in joints that did not achieve clinical success but had measurable improvement (i.e., a contracture reduction of ≥20° in the study of origin).
Methods
Patients included had participated in in JOINT I/II or CORD I (plus extension)/CORD II [21]. Patients with with Dupuytren’s Disease affecting ≥1 MP joint (contracture ≥20° to ≤100°) or 1 PIP joint (contracture ≥20° to ≤80°) were enrolled. Each treatment included a single injection of 0.58 mg CCH (maximum of 3 injections) into the cord followed by a finger extension the next day, with a 30-day follow-up. The objectives were to assess:
- recurrence of contracture in joints that had achieved clinical success in the study of origin;
- nondurability of response in joints that had showed measurable improvement in the study of origin; and
- long-term safety after CCH injection at 2- to 5-year follow-up visits.
Trial design and patient flow are included in Figure 10. Demographics and disease characteristics at baseline for CORDLESS participants were similar to those from the 5 previous CCH studies [21].
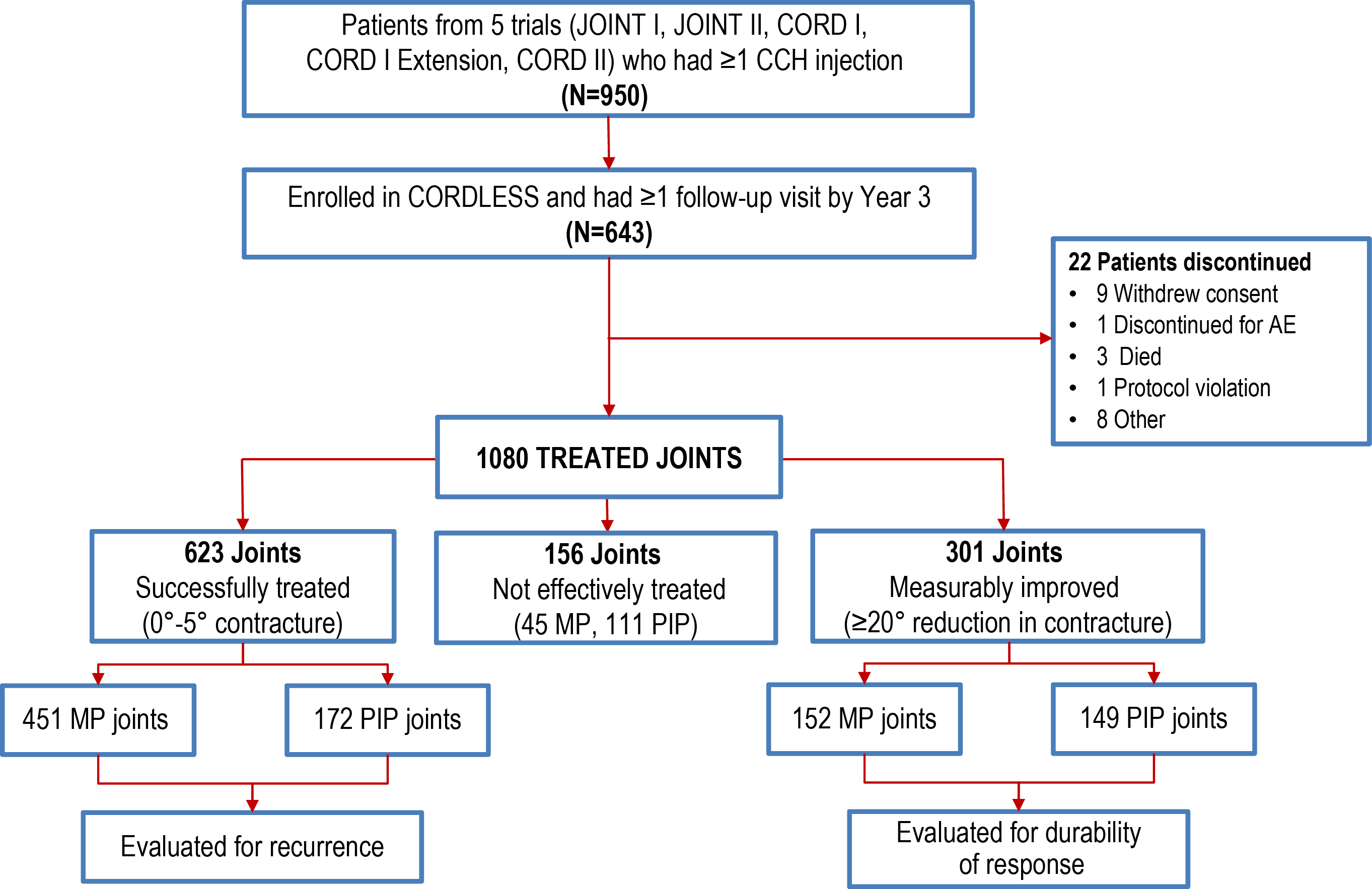
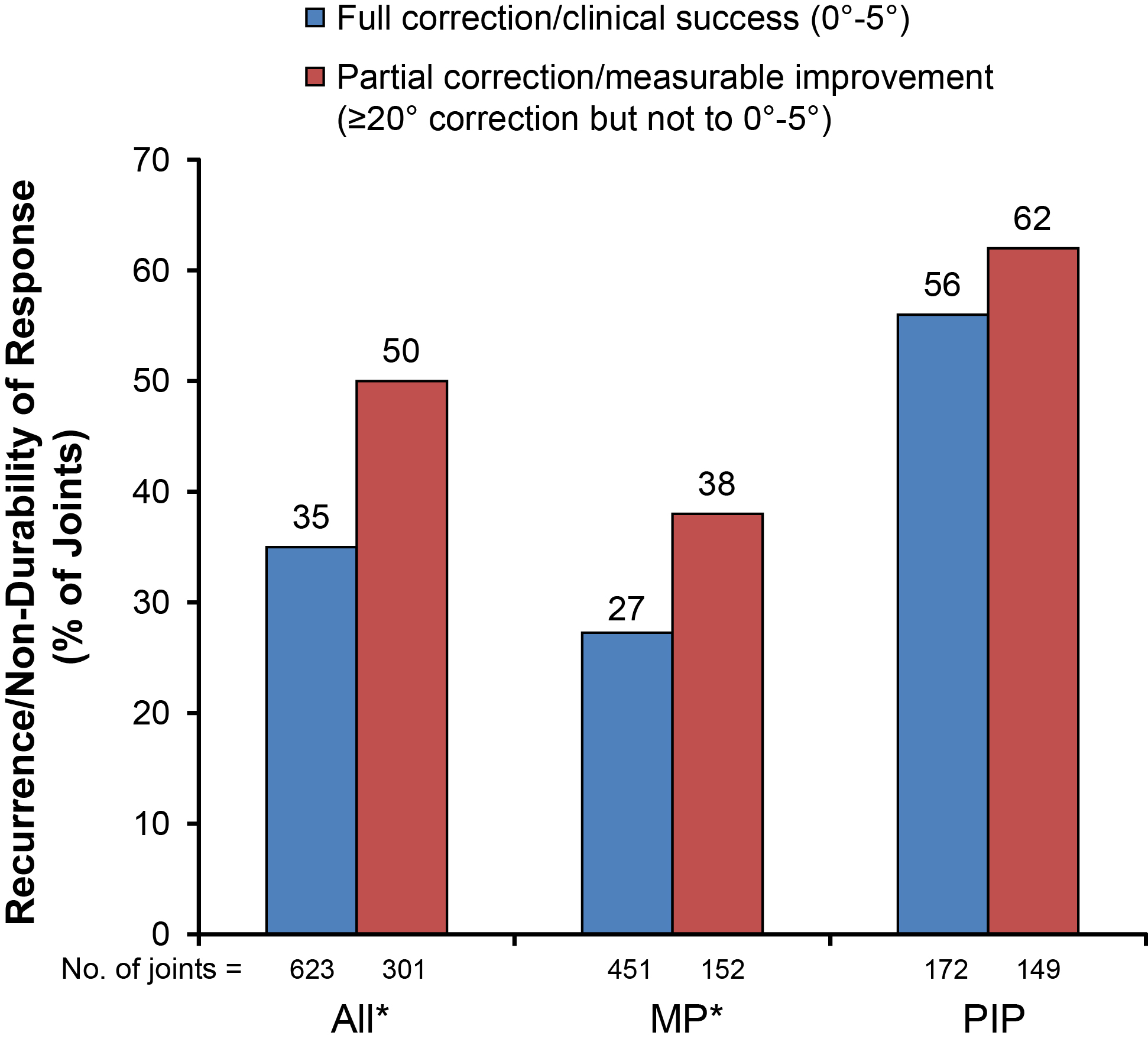
Results: successfully-treated and measurably improved patients
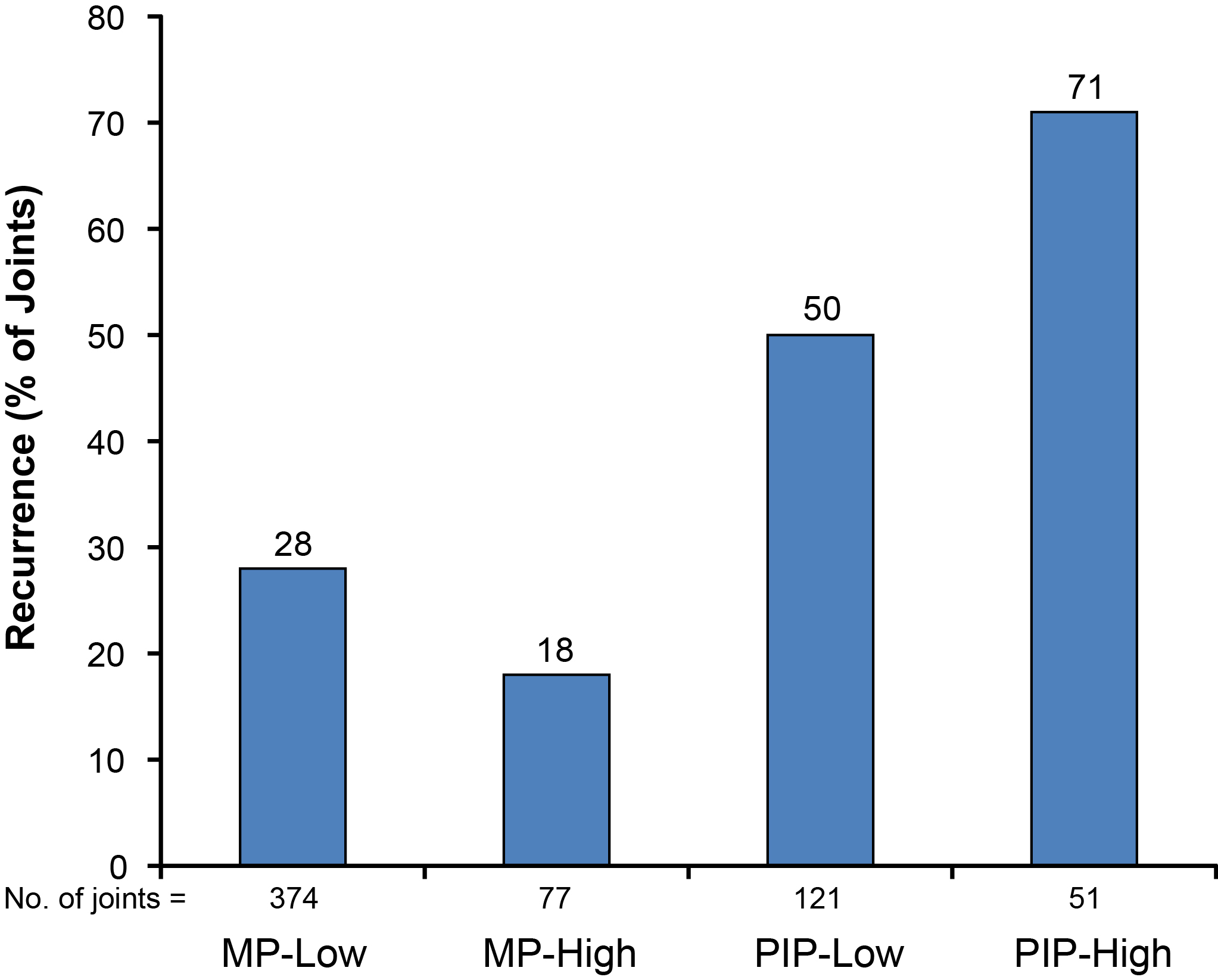
Overall, 406 successfully treated joints (65%) showed a sustained response to CCH over 3 years [21]. The recurrence rate was higher for PIP joints (56%) than MP joints (27%) (Figure 11). PIP joints showed a lower durability of response than MP joints. Figure 12 shows recurrence rates by initial severity.
Results: safety and tolerability
During the 3-year follow-up period, 193/643 (30.0%) of patients experienced 370 AEs, mostly mild or moderate (Table 2); and 31 patients (4.8%) had severe AEs, none of which were considered by the investigator to be related to treatment [21].
| N (%) | |
|---|---|
| Adverse events | 193 (30) |
| Osteoarthritis, mild | 16 (3) |
| Hypertension | 10 (2) |
| Cataract | 9 (1) |
| Atrial fibrillation | 7 (1) |
| Serious adverse event | 50 (8) |
| Atrial fibrillation | 4 (<1) |
| Small intestinal obstruction | 4 (<1) |
| Cerebrovascular accident | 3 (<1) |
| Nephrolithiasis | 3 (<1) |
| Osteoarthritis | 3 (<1) |
| Death | 3 (<1) |
Summary
Three-year data from CORDLESS showed that 65% of joints (i.e., those successfully treated with CCH) had a durable correction [21]. Three years after treatment, the overall recurrence rate, based on the objective definition used, was 35%, with a lower rate in MP joints (27%) than PIP joints (56%). Recurrence was highest in initially severely affected PIP joints (71%). PIP joints are known to be less responsive to other therapeutic interventions and to have less durable improvement. This may argue strongly for earlier treatment of PIP joints than when surgery was the single treatment option.
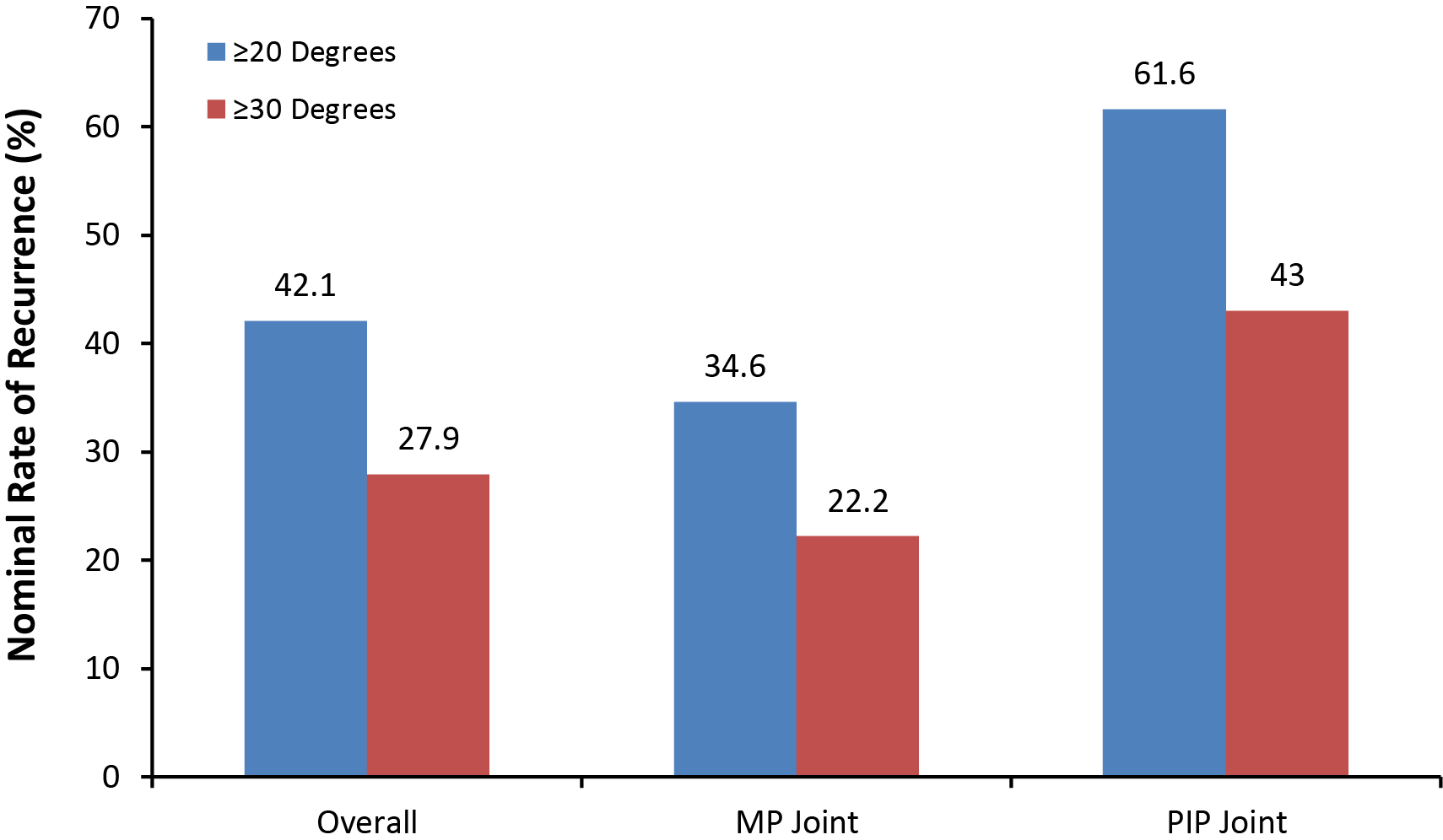
Cordless study: 4-year interim data
For the 4-year data, which are are not finalized, the nominal rates of recurrence in joints achieving clinical success were 42.1% and 27.9% for ≥20º and ≥30º worsening, respectively [27]. The recurrence rate slowed from Year 3 to 4 (7.1% increase) compared with Year 2 to 3 (15.4% increase) [27]. PIP joints showed a higher recurrence rate than MP joints (Figure 13) [27]. Recurrence rate for low severity PIP joints (<40º) was 58% while the recurrence rate for high severity PIP joints (≥40°) was 71% [27]. Currently, a total of 543 (87.2%) of successfully treated joints have not had additional medical/surgical interventions [27]. From Year 3 to Year 4, the rate of CCH use for the treatment of worsening contractures in joints with clinical success surpassed the rate of secondary fasciectomy (Table 3). No long-term safety/risk issues were identified [27].
| Intervention | Year 2 n (%) |
Year 3 n (%) |
Year 4 n (%) |
|---|---|---|---|
| Total interventions | 15 (100%) | 32 (100%) | 38 (100%) |
| CCH | 0 (0%) | 6 (18.8%) | 18 (47.4%) |
| Fasciectomy | 9 (60%) | 20 (62.5%) | 12 (31.6%) |
| Needle aponeurotomy | 3 (20%) | 4 (12.5%) | 5 (13.2%) |
| Fasciotomy | 0 (0%) | 1 (3.1%) | 1 (2.6%) |
| Dermofasciectomy | 0 (0%) | 1 (3.1%) | 0 (0%) |
| Other | 3 (20%) | 0 (0%) | 2 (5.3%) |
8-year follow-up data/phase 2 trial
In a phase 2 clinical trial of injectable collagenase designed to determine dose response, efficacy, and safety, subjects were randomized to receive placebo, 2,500 U, 5,000 U, or 10,000 U of collagenase as a single injection [13]. Eight subjects participated in an 8-year follow-up to this study. Average age at 8-year follow-up examination was 69 years (range, 52–86). Average age at initial diagnosis of Dupuytren’s Disease was 44 years (range, 30–66) [28].
MP and PIP contractures
Six patients had been treated for isolated MP joint contracture. Average pre-injection contracture was 57°; average contracture was 9° at 1 week, 11° at 1 year, and 22° (range, 0°–55°) at 8-year follow-up. Four of 6 patients experienced recurrence, whereas 2/6 had no evidence of disease recurrence at 8 years [28]. Two patients were treated for isolated PIP contracture. Pre-injection contractures were 35° and 55° in the 2 subjects in the PIP group, respectively. These contractures were 0° and 15° at 1 week, 0° and 25° at 1 year, and 50° and 70° at 8-year follow-up. Both patients experienced disease recurrence [28].
One-year post-marketing data
A search of safety data for AEs received by the CCH marketing sponsor (Auxilium Pharmaceuticals, Chesterbrook, PA, USA) during the first 12 months after US approval, February 3, 2010, through February 2, 2011, was conducted [29]. Reporting rates are the number of spontaneous AE reports received by the manufacturer for the population at risk (i.e., patients treated/exposed to the product; ~5,400 injections in the period, based on distribution records) during this initial 1-year period.
During the first post-marketing year, a total of 270 AEs were reported in 115 patients and were similar in type and severity to those reported in CCH clinical trials [29]. Based on these data, no safety-related changes were made to the FDA-approved product label. Of the 270 AEs received, skin tears (13%), peripheral edema in the extremity (11%), and local contusion (9.6%) were the most prevalent. A total of 35 skin tears were reported, all of which occurred during the finger extension procedure; most healed without intervention [29]. Additional AEs representing >2% of the total post-marketing reported events are presented inTable 4, along with reporting rates by AE.
| # of reported Aes | Post-marketing AEs (%)a | Reporting rateb per 1,000 doses |
|---|---|---|
| Skin tear (35) | 13.0 | 6.5 |
| Peripheral edema (30) | 11.1 | 5.6 |
| Contusion (26) | 9.6 | 4.8 |
| Drug ineffective (13) | 4.8 | 2.4 |
| Injection-site hematoma (10) | 3.7 | 1.9 |
| Lymphadenopathy (8) | 3.0 | 1.5 |
| Pain in extremity (8) | 3.0 | 1.5 |
| Blood blister (8) | 3.0 | 1.5 |
| Injection site pain (7) | 2.6 | 1.3 |
| Tenderness (6) | 2.2 | 1.1 |
| aTwo hundred seventy total adverse events reported bApproximately 5,400 injections in the current analysis |
||
During the first post-marketing year for CCH, the AEs reported were similar in type and severity to those reported in clinical trials [29]. No safety-related changes needed to be made to the product label since local, nonserious reactions to treatment were most commonly reported, and serious AEs associated with CCH were reported infrequently and were less common than the documented major complications reported from surgical treatments.
Clinical considerations and commentary
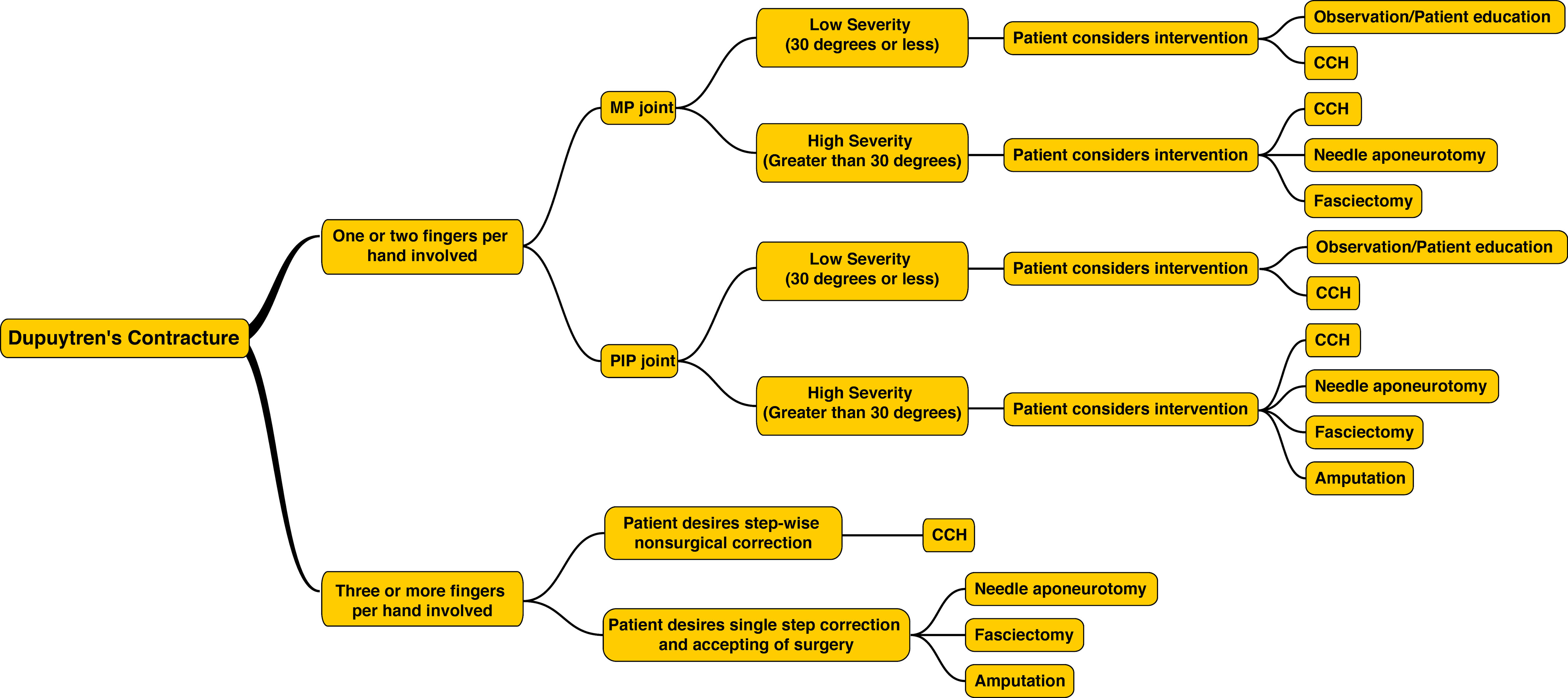
Figure 14 presents a CCH treatment algorithm, illustrating where enzyme injection is likely to contribute to effective management of Dupuytren’s contracture.
CCH dosing, administration, and treatment
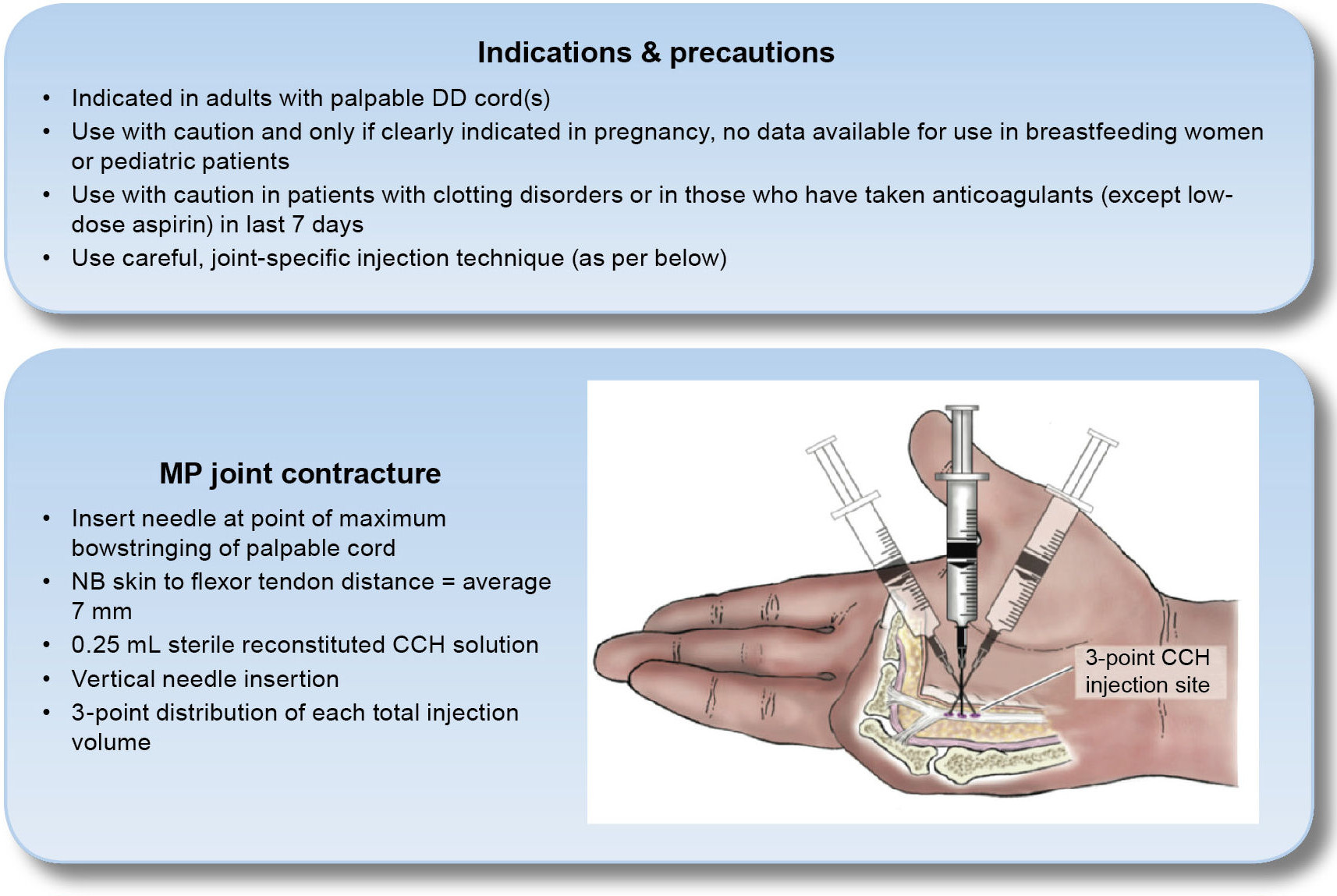
The manufacturer-recommended injection procedures are described in this section with added clinical considerations from the author; clinical techniques will be presented in the Case Study images and videos at the end of this chapter.
The dose of CCH is 0.58 mg per injection into a palpable cord with a contracture of a MP joint or a PIP joint [1].
Using a new 1 mL hubless syringe that contains 0.01 mL graduations with a permanently fixed, 27-gauge ½-inch needle, withdraw a volume of reconstituted solution (containing 0.58 mg of CCH) as follows [1]:
- 0.25 mL for cords affecting a MP joint
- 0.20 mL for cords affecting a PIP joint
Instructions regarding CCH injection technique are provided in Figure 15 and in each of the Case studies.
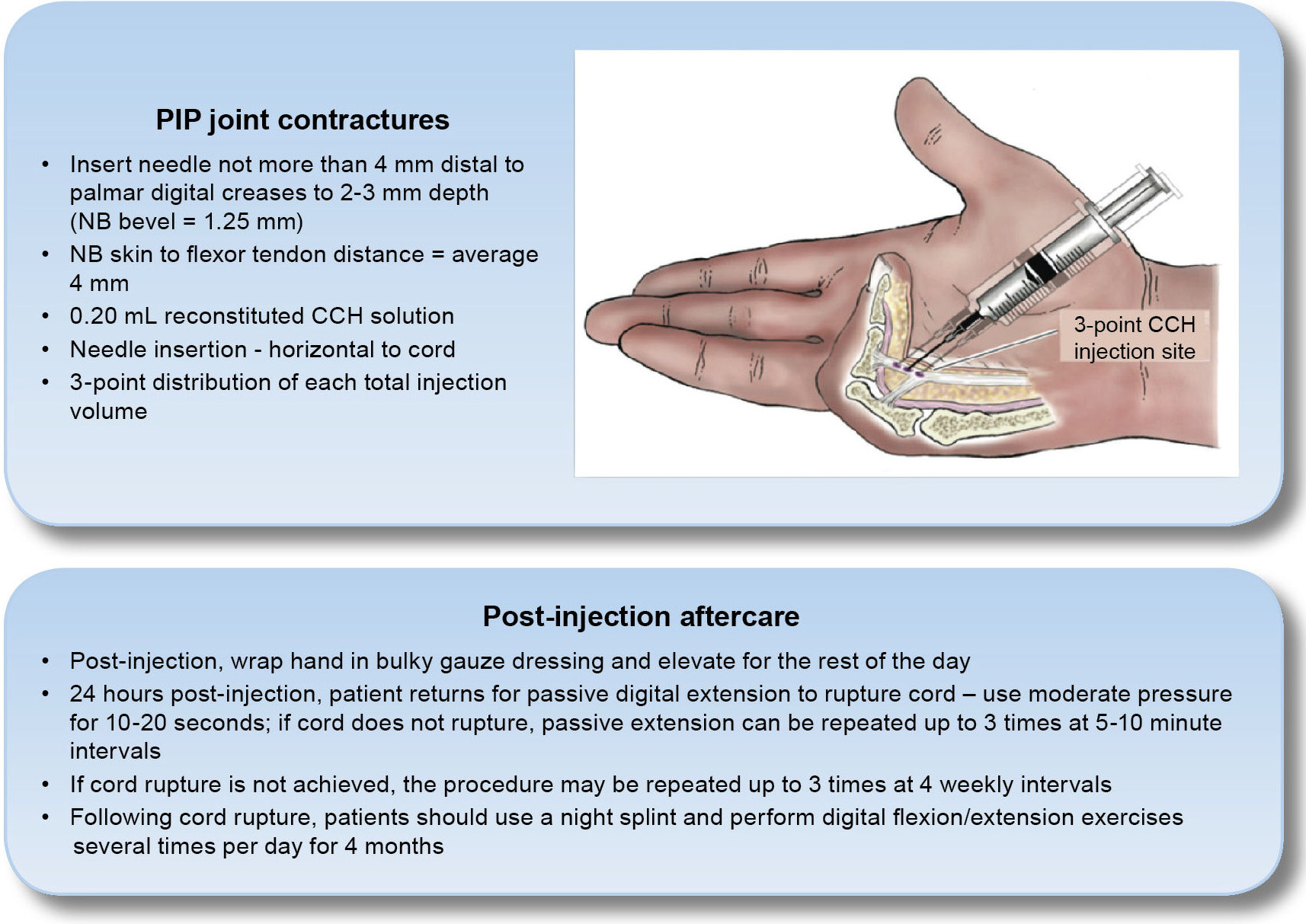
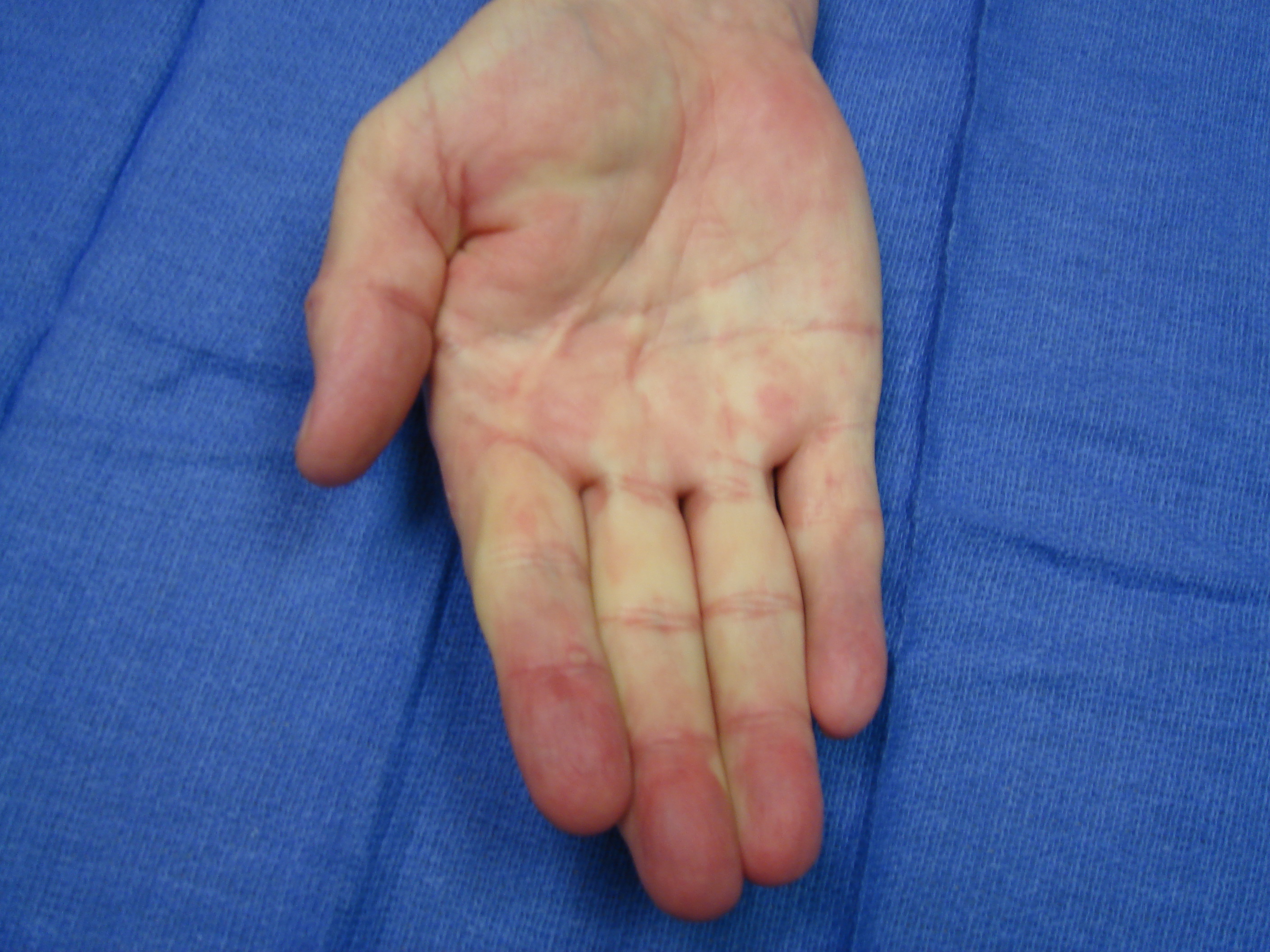
Finger extension procedure [1]
If any contracture remains at the follow-up visit after enzyme injection, a passive finger extension procedure is performed: local anesthesia should be used before manipulation. Generally, a dose of 4 to 6 mL of local anesthetic is instilled in the palm, flexor sheath, and interdigital tissues; advise the patient you will leave the room (for 10 minutes) to allow the medication to fully take effect (see Case study images and videos).
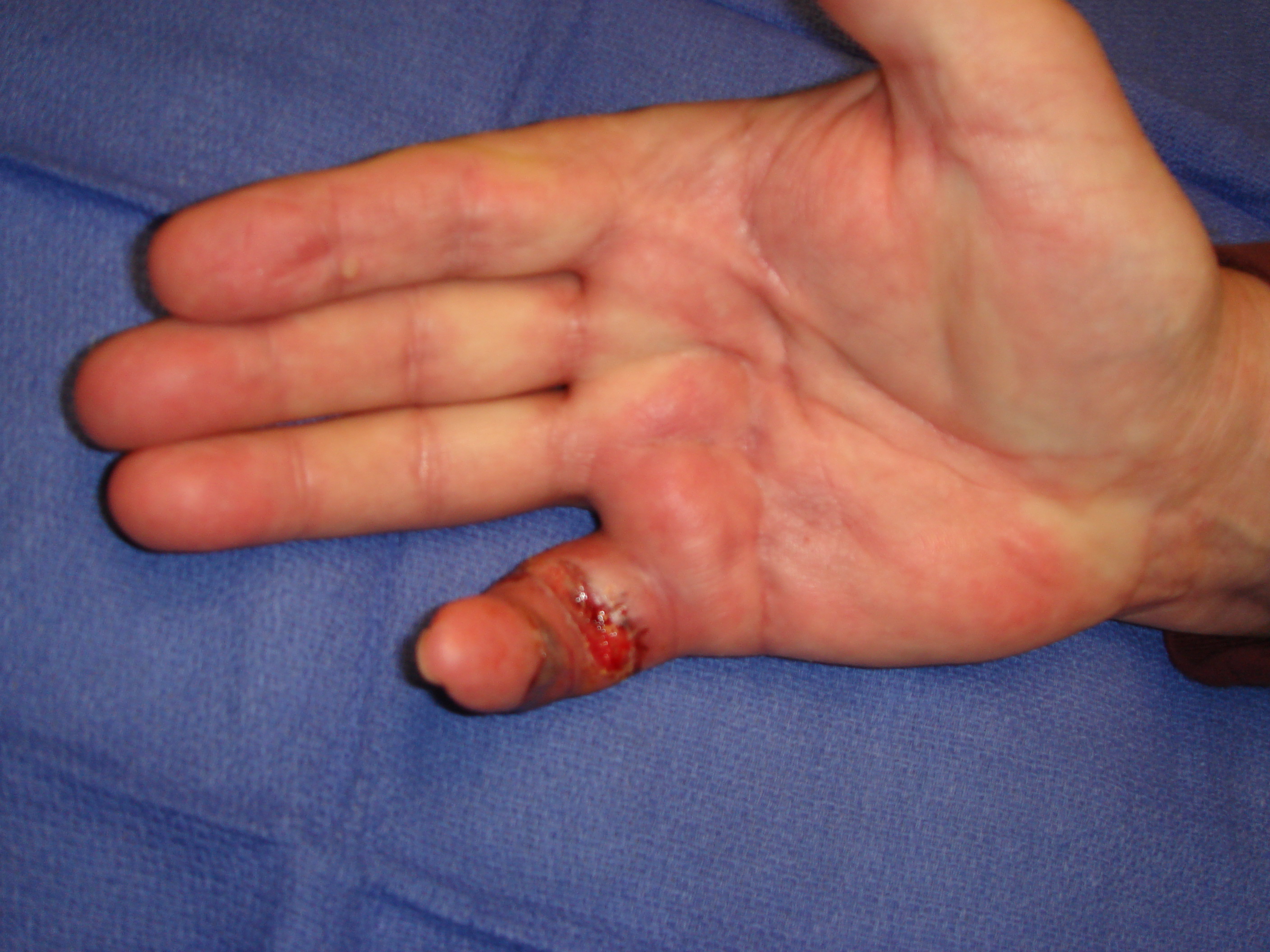
When the patient is entirely numb and comfortable (and given a “safe word” if pain occurs, to stop the manipulation), support the wrist on the exam table and apply increasing stretching to the finger/cord by extending the finger for ~10 to 20 seconds. For cords affecting the PIP joint, one generally does this with the MP joint mildly flexed. As some patients may experience skin splitting/tears, cover the area with gauze while manipulating. The bloody exudate from a tear will be a combination of blood, edema fluid, and injected anesthetic; and it will likely soak several gauze pads.
If the first finger extension procedure does not result in disruption of the cord, a second and third attempt can be performed. However, it is most important that the patient is comfortable and pain-free for correction to be maximized. Add anesthetic if the patient is not comfortable. It is most unlikely post-collagenase that the cord will not rupture with the scenario of a numb hand and persisting extension by the physician. Once extended, palpate the former zone of contracture to assure cord disruption. If there has been an interdigital (“natatory”) cord or combined central and abductor cord, this is a good time to manipulate (again, if needed) to and break those residua, and to passively extend and abduct all the fingers.
Next, have the patient flex and extend. With longstanding PIP joint contractures, the active extension will not likely equal passive correction. It is important that the patient notices this difference and understands the emphasis on both nightly splint correction and attention to regaining PIP joint extensor pull. In the very unlikely event that the cord has not been disrupted after 3 attempts, a follow-up visit may be scheduled in ~4 weeks. At that subsequent visit, an additional treatment cycle or a surgical alternative may be considered. These approaches likewise may be considered for partial corrections or if there are secondary or additional (ipsilateral or contralateral) contractures.
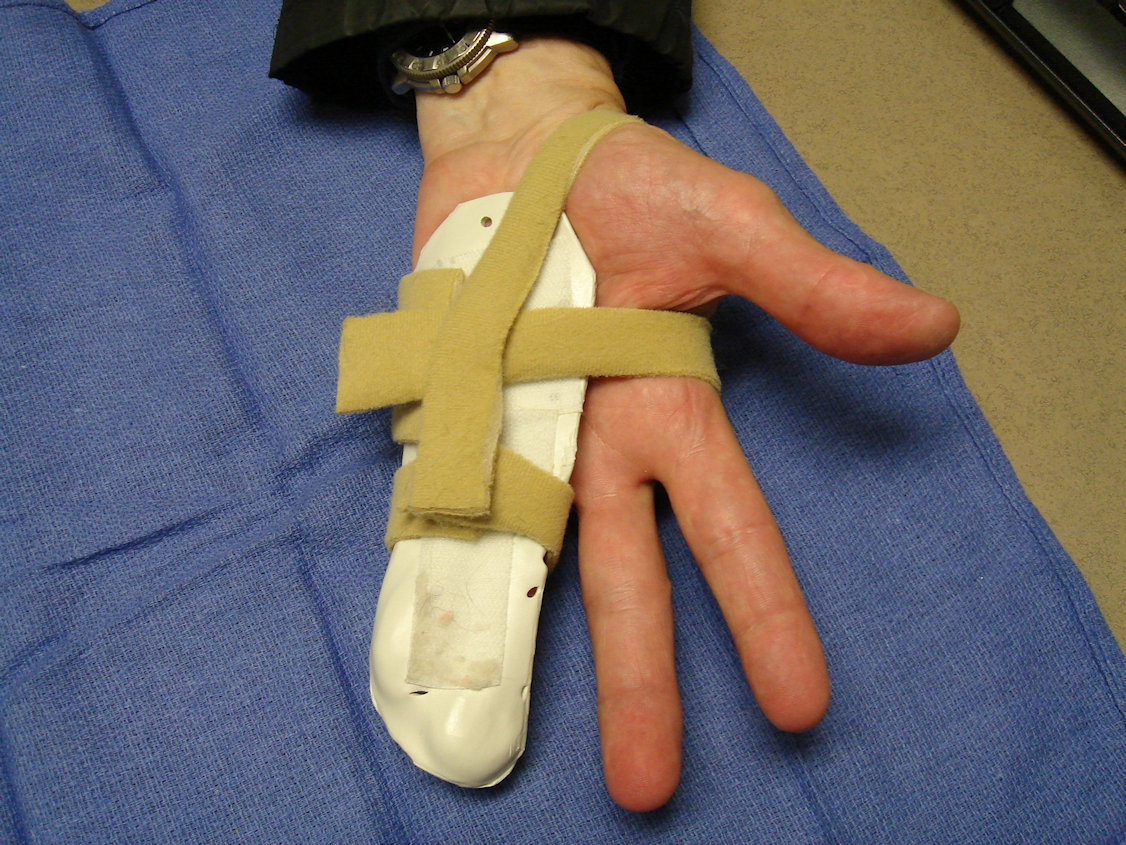
Following the finger extension procedure, fit the patient with a dorsal- or volar-based finger or hand splint to maintain maximal extension, and provide instructions for nightly use at bedtime for ~3 months. Instruct the patient to perform finger extension and flexion exercises several times daily and to not wear the splint full-time. Most of our patients have not required therapy services beyond custom thermoplastic splinting; but significant active PIP extension deficiency is important to address. Those with skin tears will do better with added dressing instruction and assistance during the next 10 to 15 days. We require that patients bring their splints to every office visit so that adjustments may be made, as needed, as swelling resolves.
Care precautions
To avoid iatrogenic flexor tendon rupture, the recommended technique of administration is to inject CCH only into the pathologic fascial cord, avoiding the tendon sheath and tendons. When injecting a cord affecting a PIP joint of the finger, the needle insertion should not be more than 2 to 3 mm in depth. Also, one must take care to inject aiming away from the tendon/sheath when distal to the palmar digital crease [1].
The bevel of a standard 27-gauge needle is ~1.3 mm, and the distance between the skin and the flexor tendon averages 7 mm at the MP joint and 4 mm at the PIP joint. Therefore, when treating finger PIP joint contracture, the cord is most safely injected more proximally, between the PIP and the MP joint flexion creases; if injecting in the finger, one inserts radial to an ulnar cord and from ulnar to a radial cord (see Case Study videos). The syringe can be stabilized with 1 hand while the other pushes the plunger to minimize the risk that the needle tip will migrate through the cord into vital structures [20].
Summary
CCH is the first significantly effective and well tolerated nonsurgical treatment of flexion contractures caused by Dupuytren’s Disease. CCH enzymatically disrupts the contracted cord while having no deleterious effect on grip strength or active flexion. CCH is effective in reducing contracture of both MP and PIP joints and in contractures of high or low severity. As CCH is administered in the physician’s office, most patients report satisfaction with treatment and rapid return to activities of daily living.
Acknowledgment
The author thanks Leonard Lionnet, PhD, of MedVal Scientific Information Services, LLC, for providing medical writing and editorial assistance.
Conflict of interest
Dr. Peimer is an advisor/consultant and speaker for Auxilium Pharmaceuticals (includes support for travel). His institution has also received grants from Auxilium Pharmaceuticals.
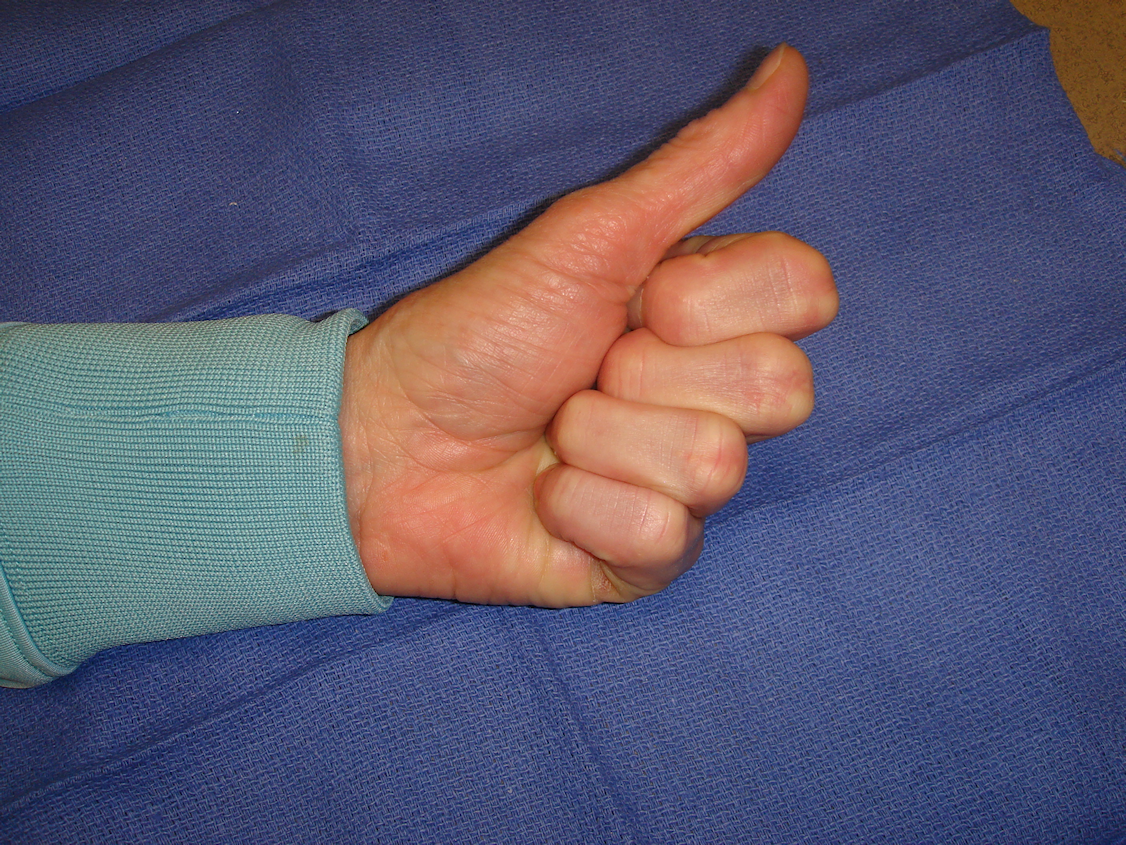
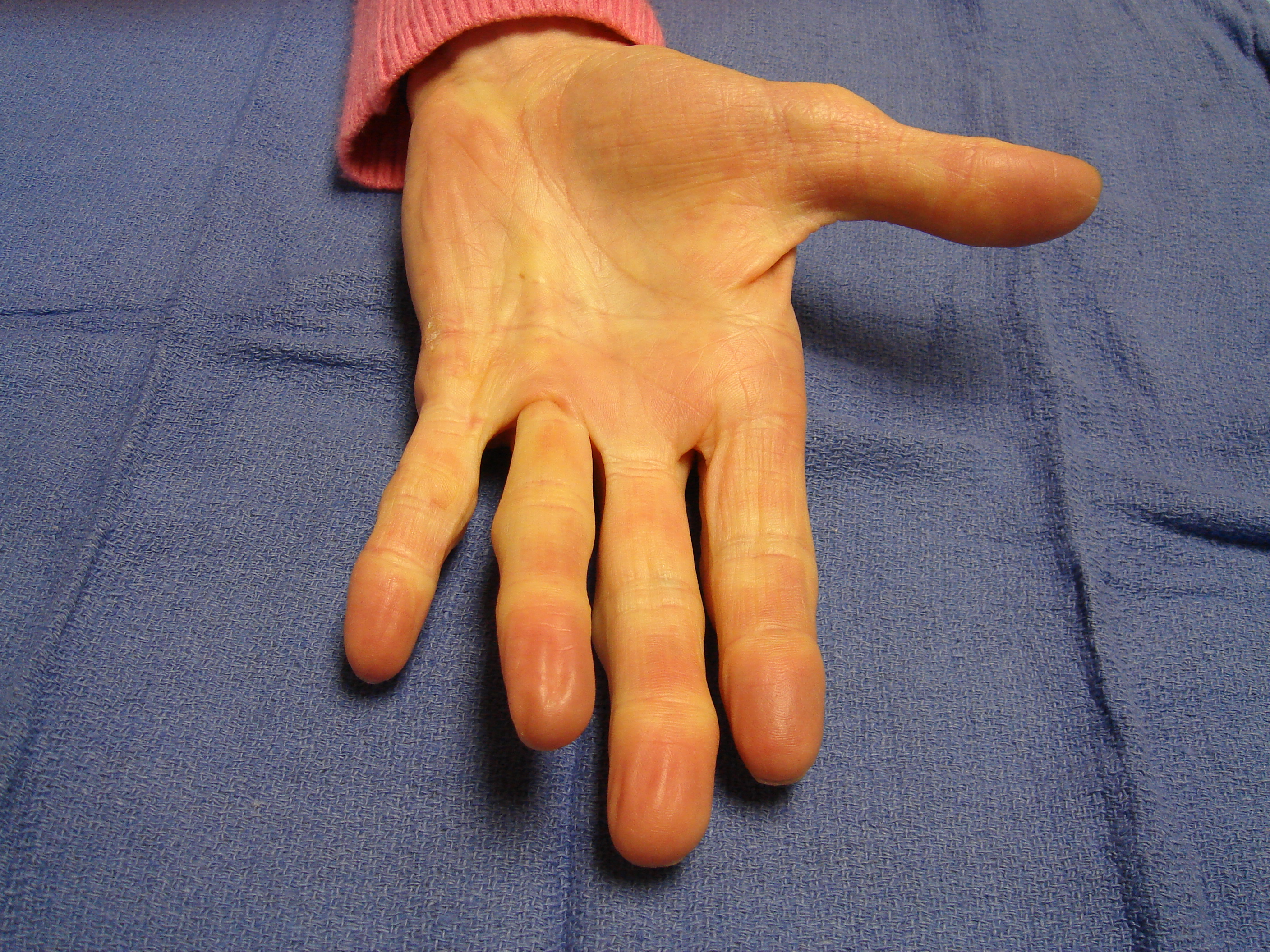
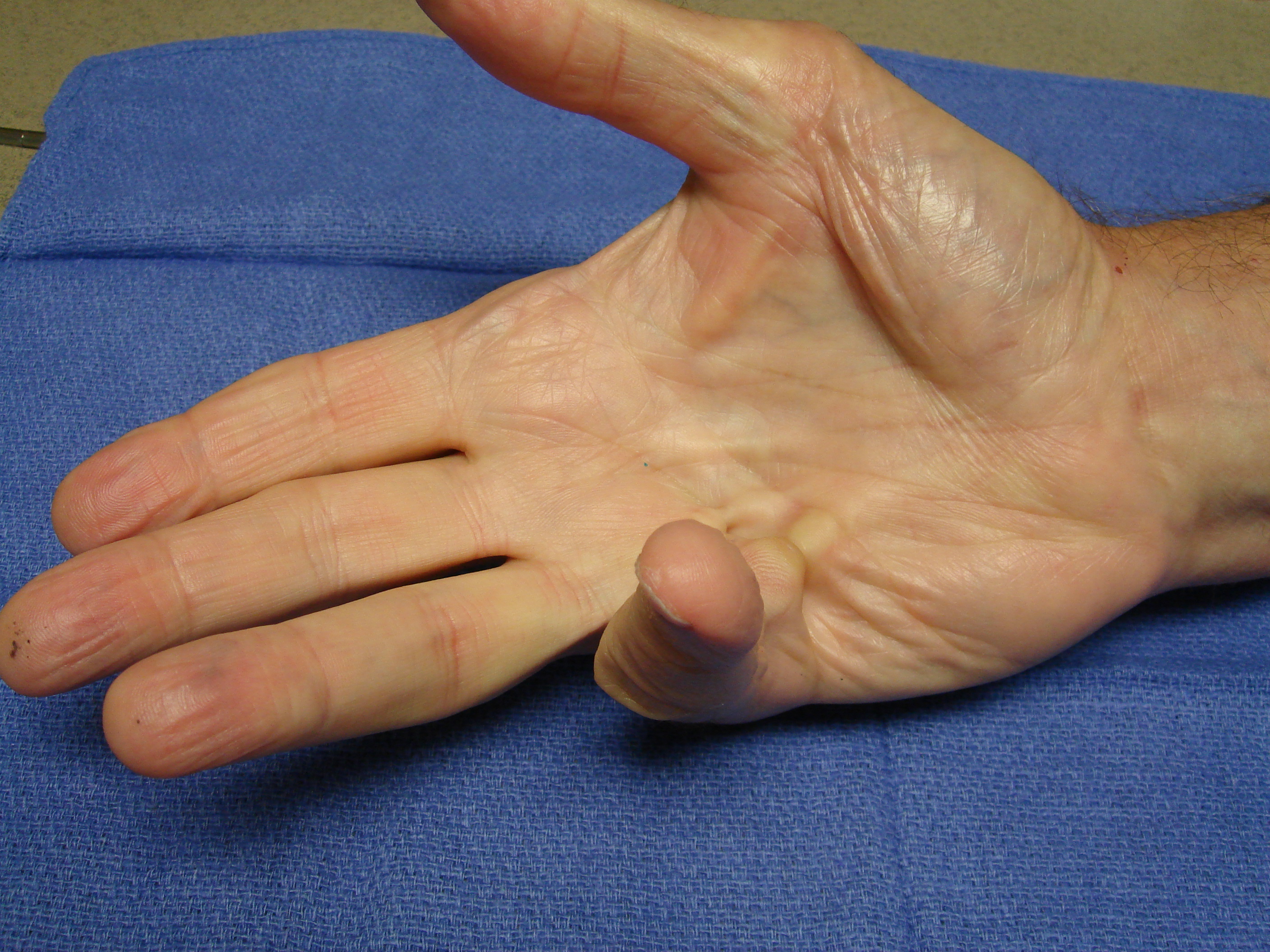
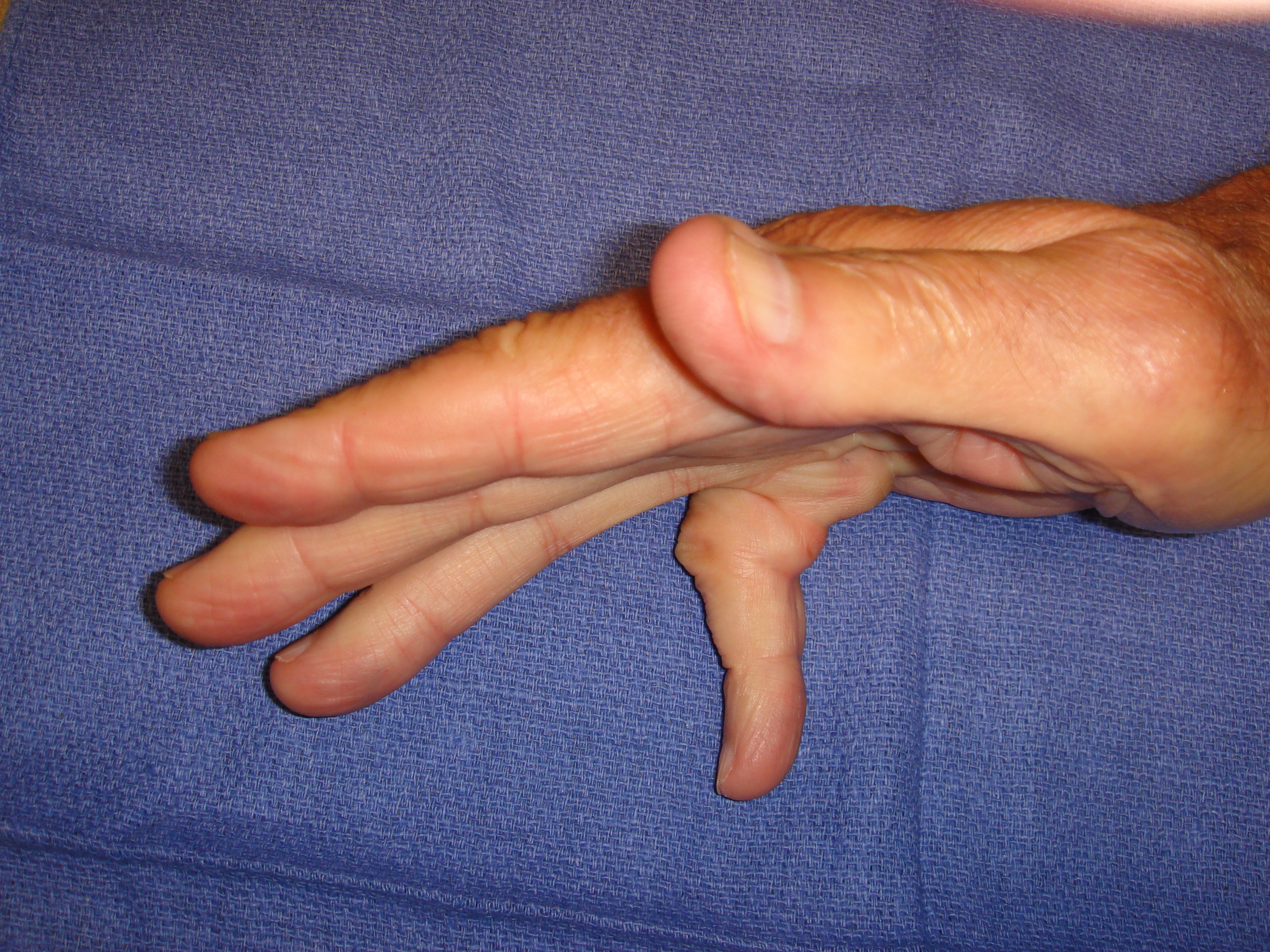
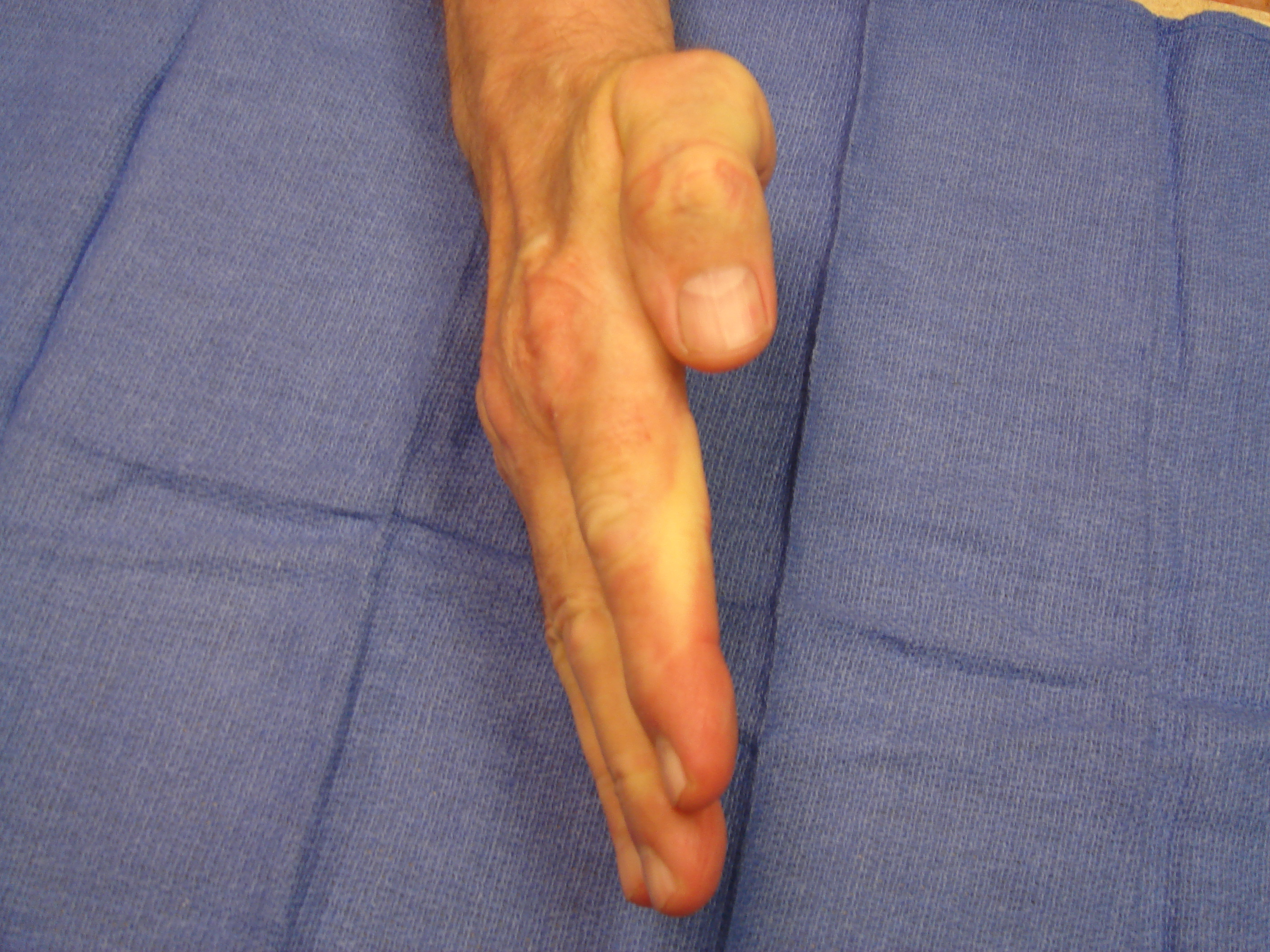
Case studies
Each patient with Dupuytren’s contracture presents individual anatomy, anatomical, and functional issues that need to be addressed (whether by collagenase or surgery). Each of these cases will illustrate different aspects of treatment and will highlight specific issues with respect to technique and care.
Case #1
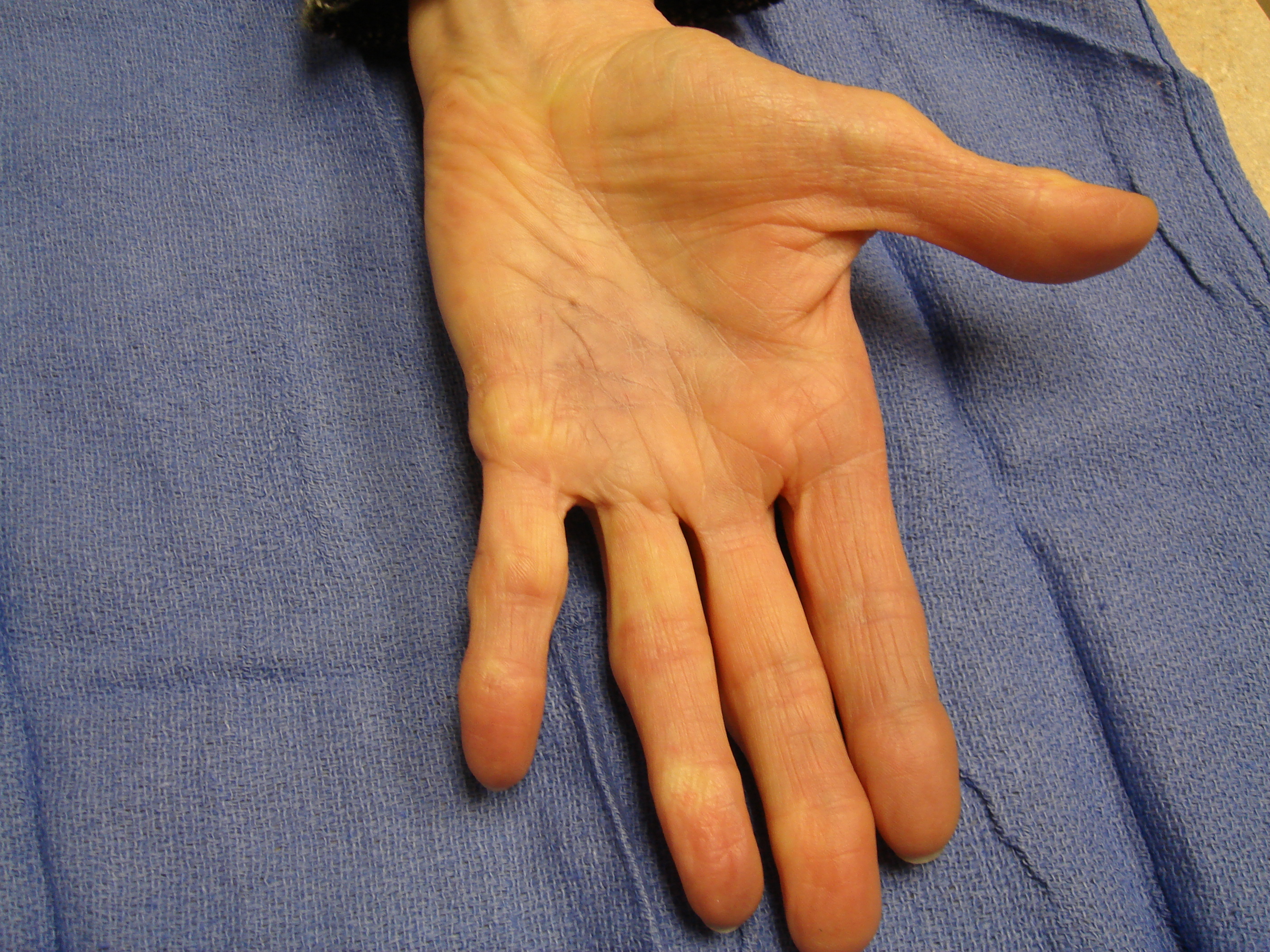
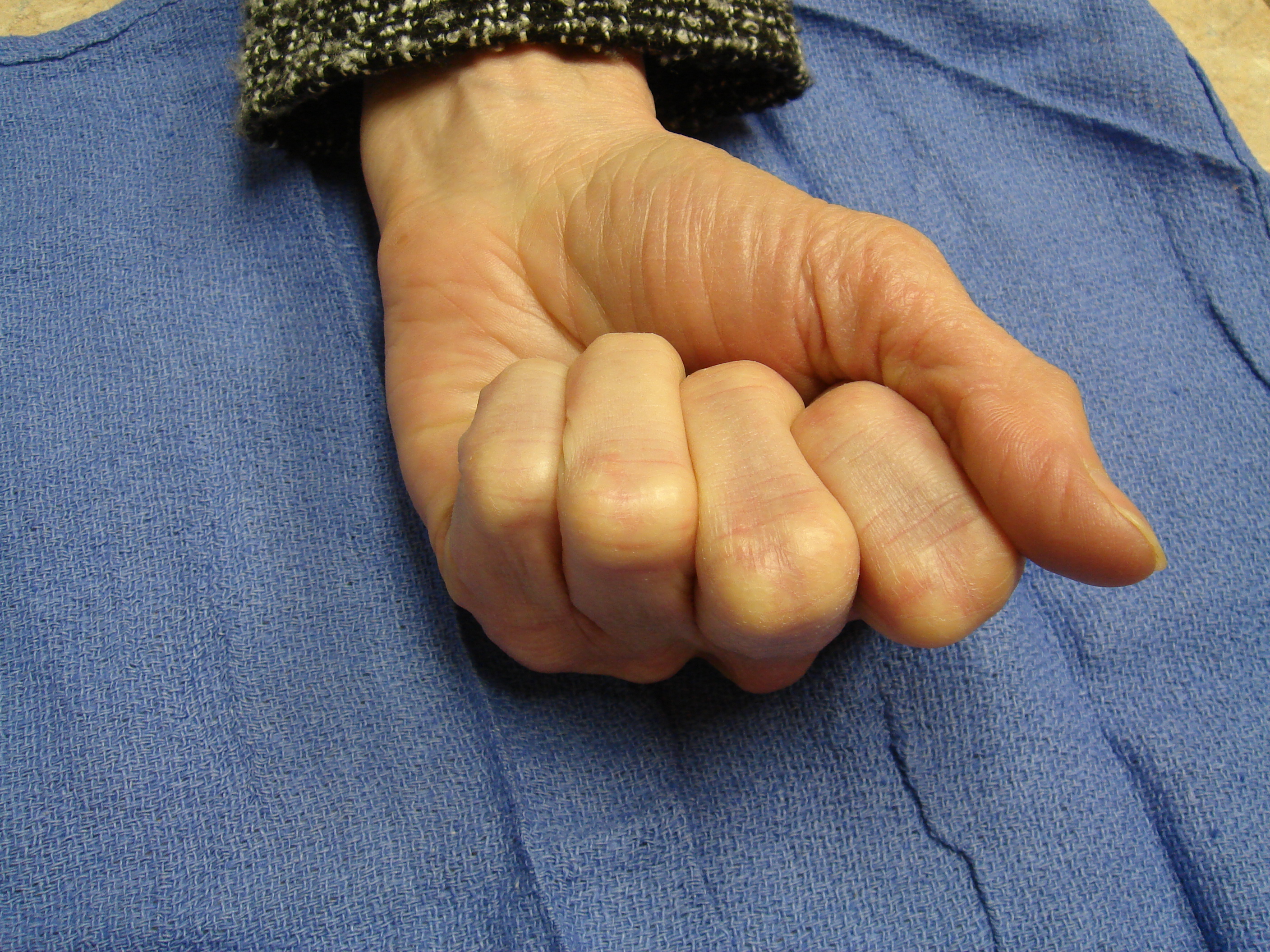
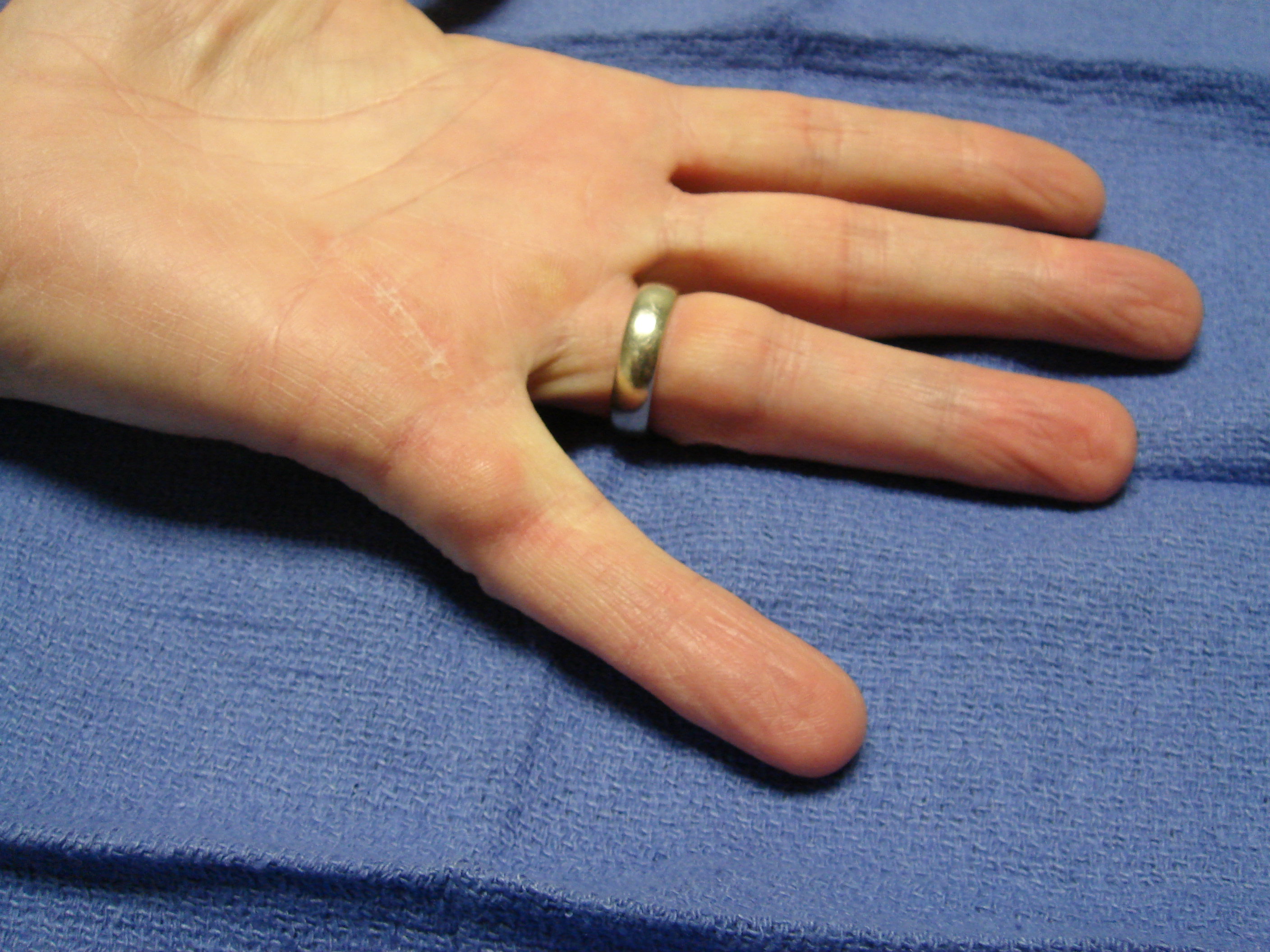
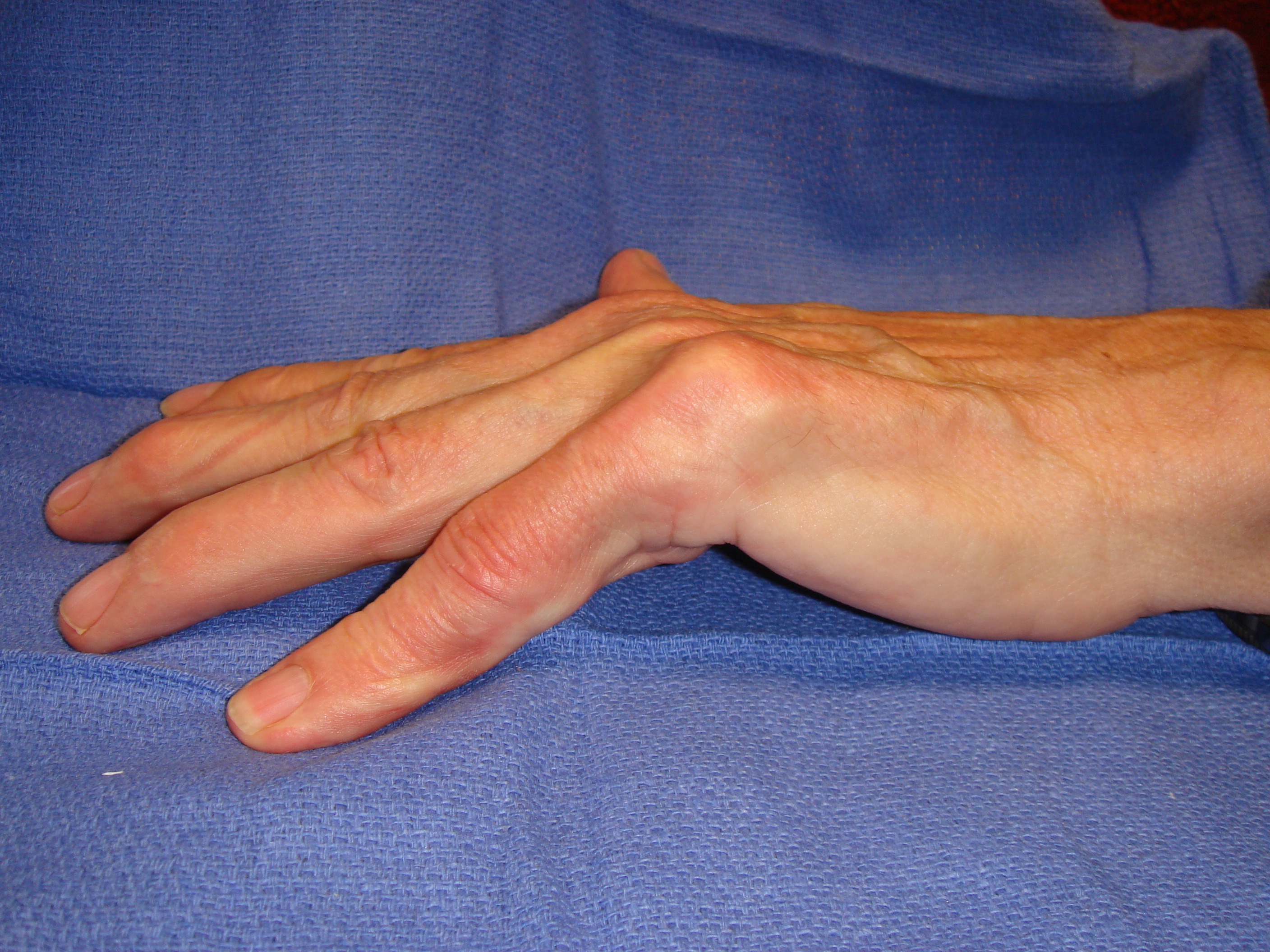
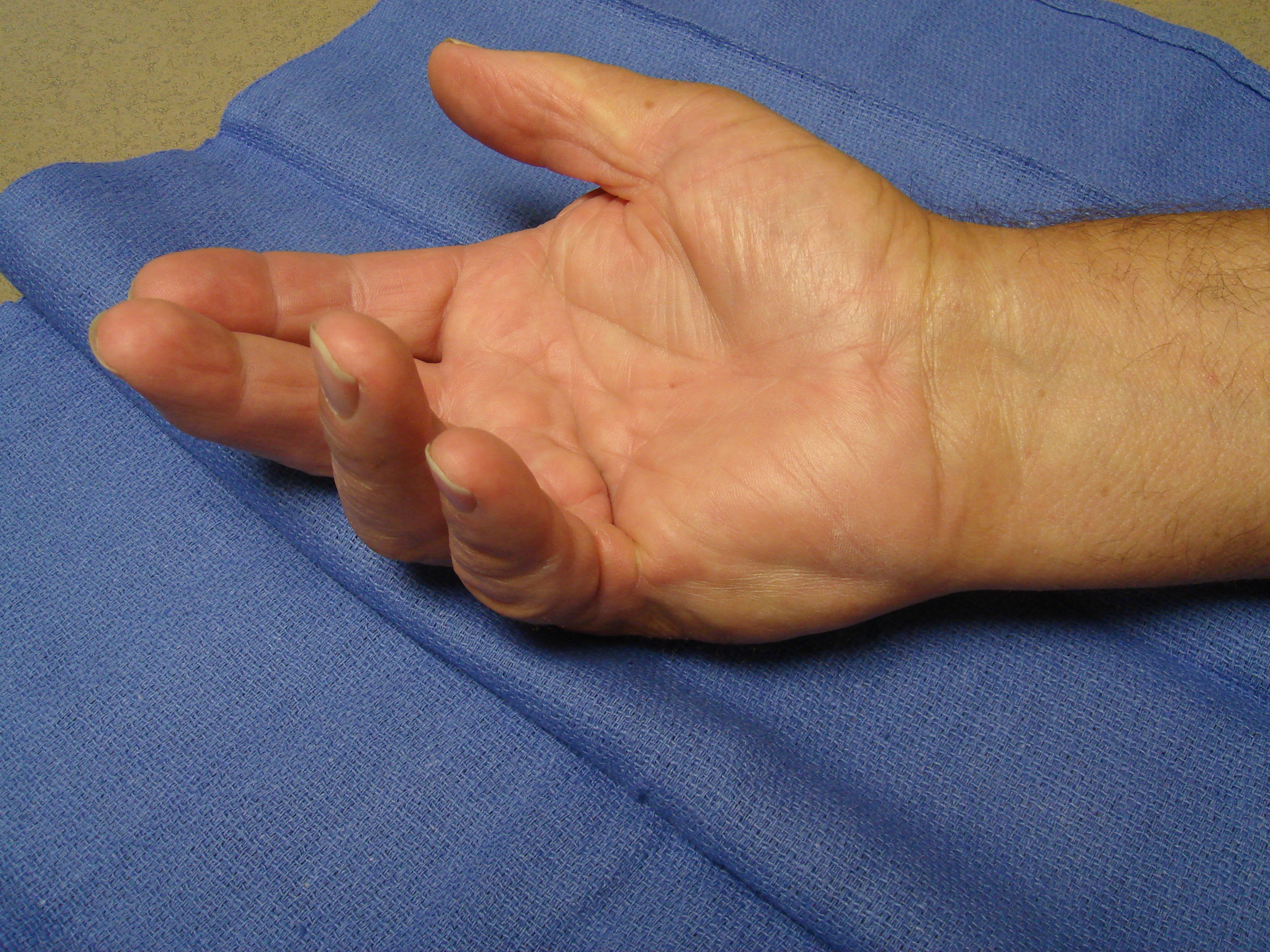
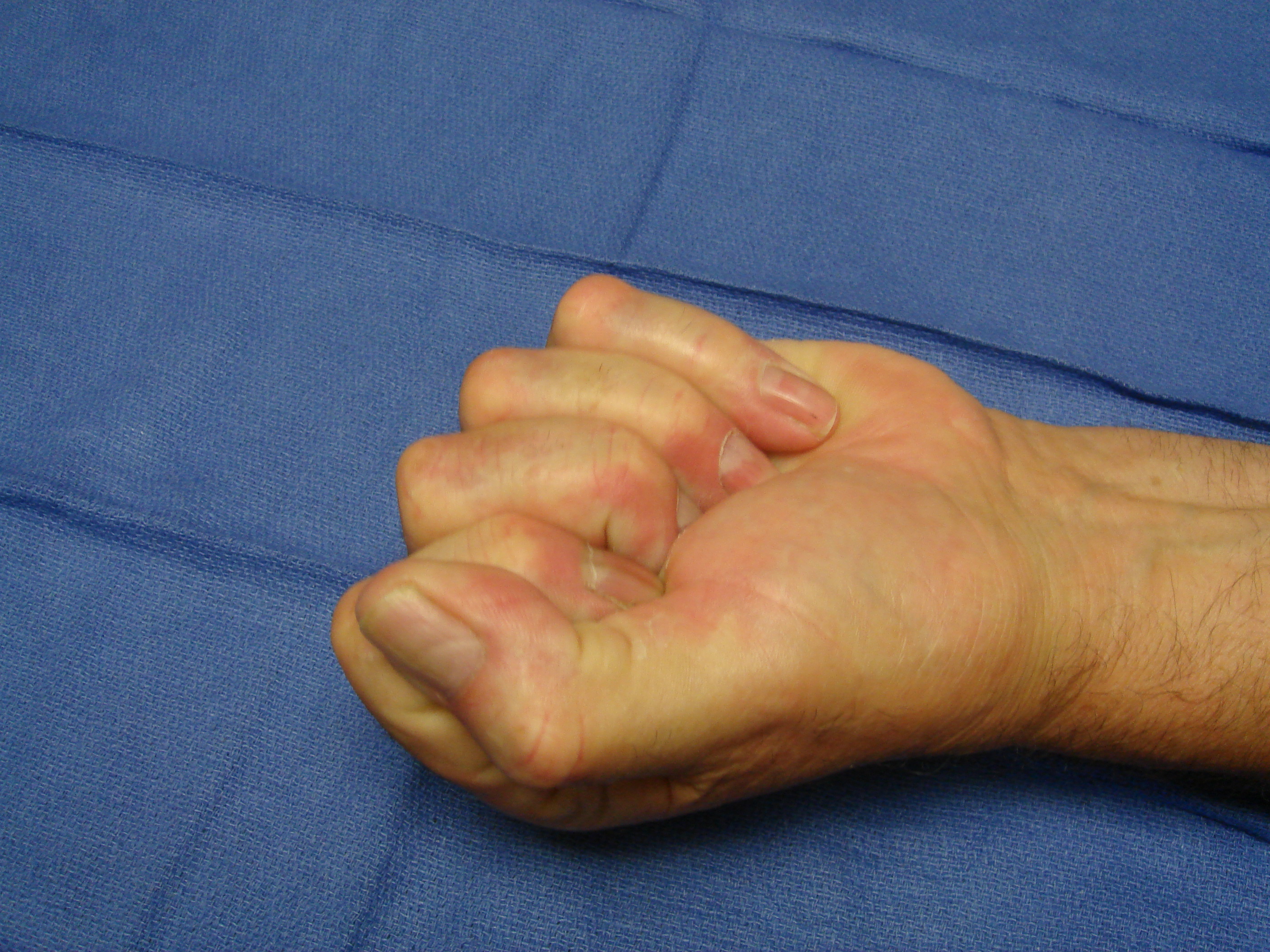
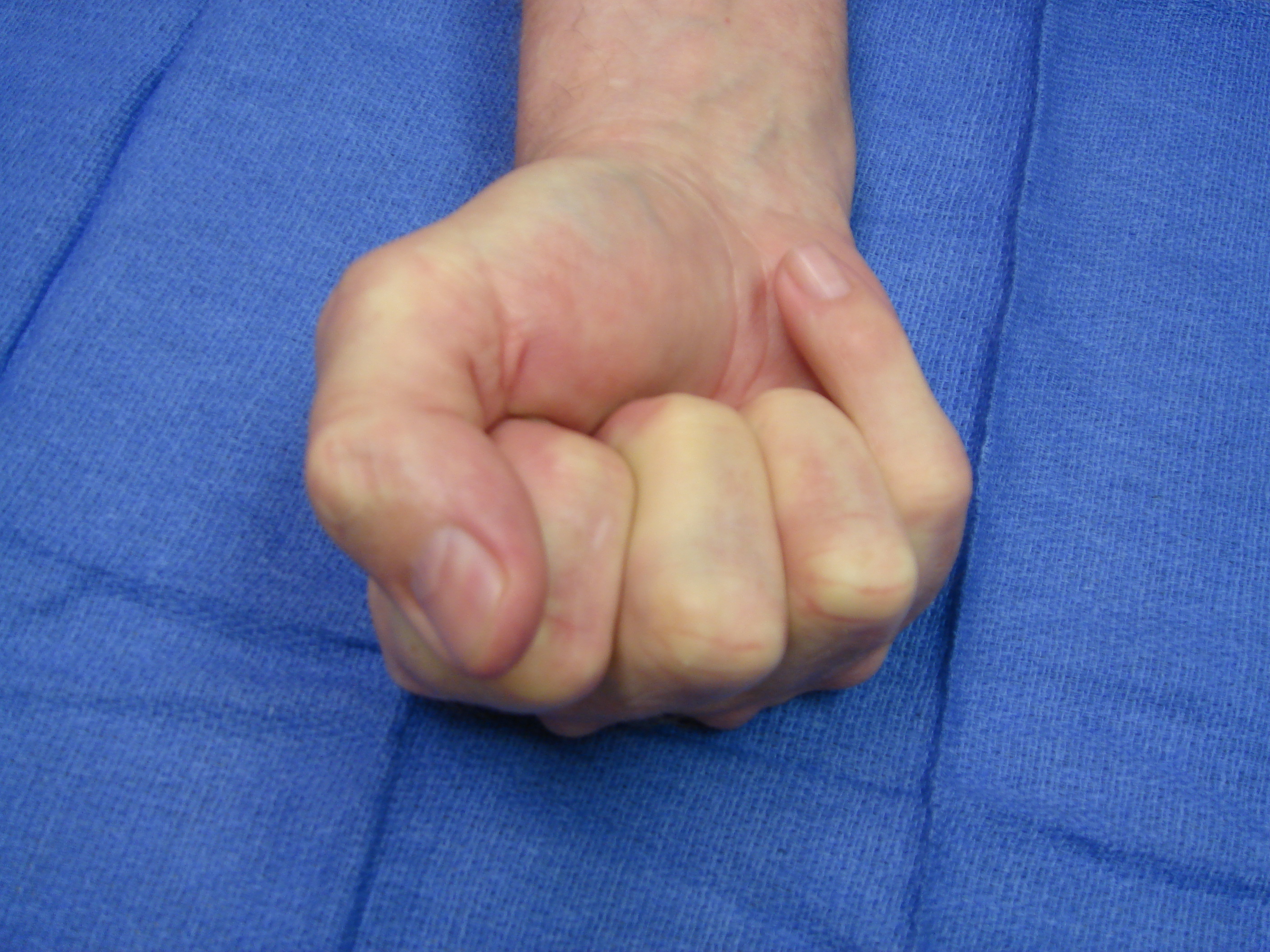
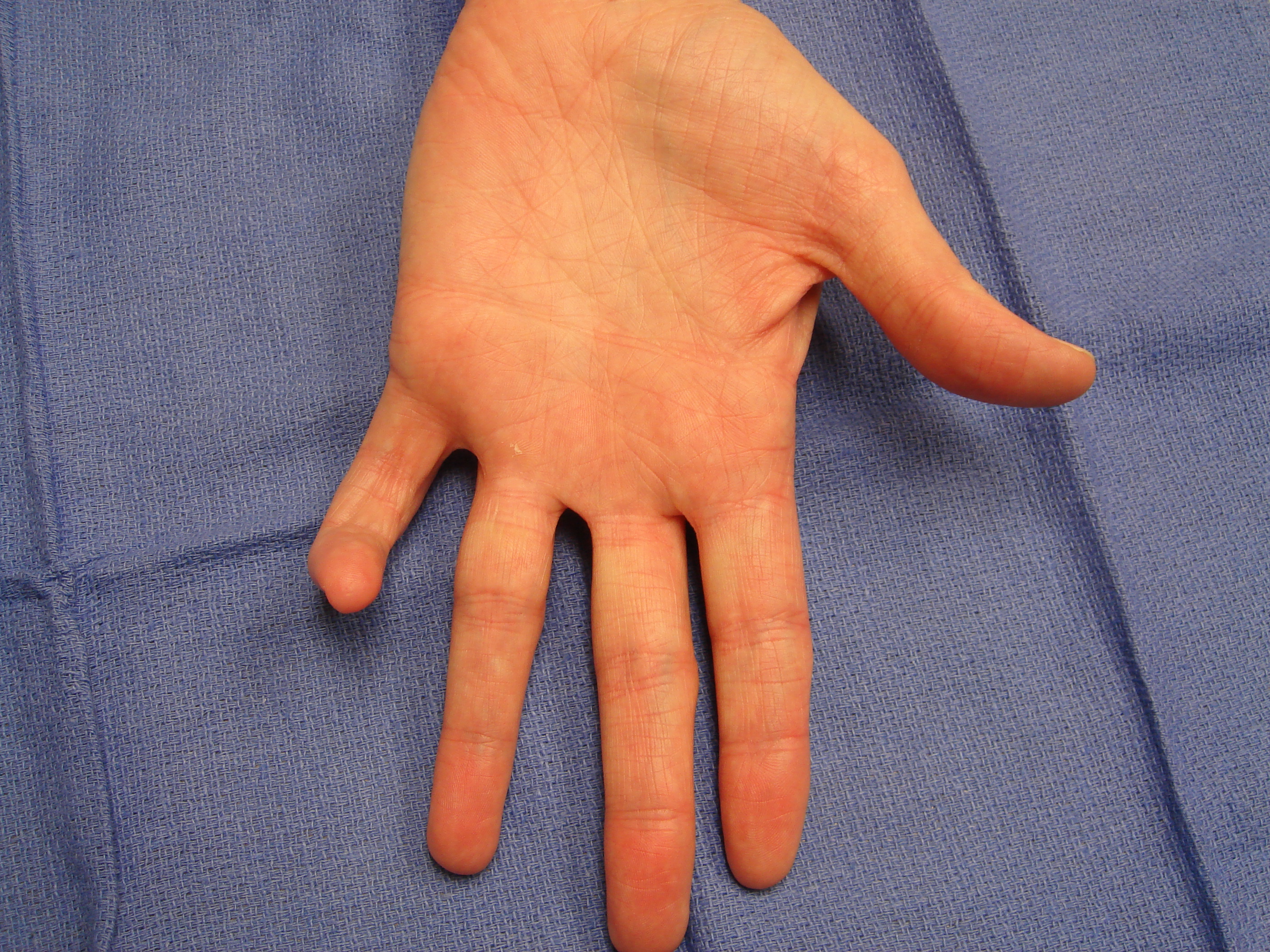
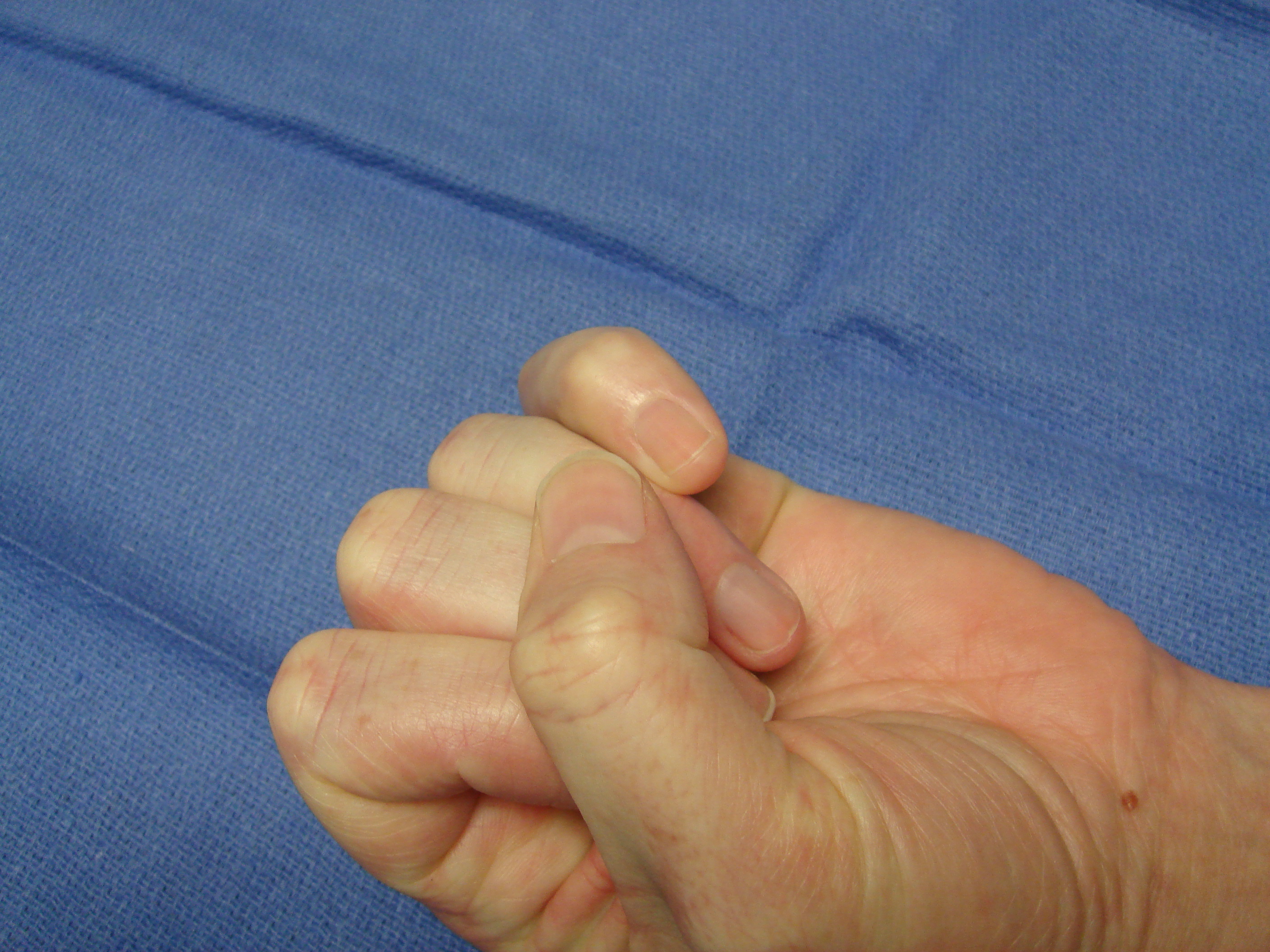
Female with contractures of her left ring and little fingers. The little finger was treated first – by our mutual decision – and then the adjacent ring finger ~9 months later.


Video 1a: Collagenase enzyme was injected into the interconnecting fourth and fifth ray plus
the independent abductor cord in the little finger (DOI: 10.4126/FRL01-006409579).
Video 1b: The manipulation was done at 48 hours, after anesthetic administration
(DOI: 10.4126/FRL01-006409581).



Case #2
Video 2a: The enzyme injection was into all intersecting cords (DOI: 10.4126/FRL01-006409584).
Video 2b: Manipulation after anesthetic administration at 48 hours produced correction for both
the fourth and fifth rays along with a small distal palmar skin tear (DOI: 10.4126/FRL01-006409587).




Case #3



Video 3a: This shows post-anesthetic manipulation at 48 hours after enzyme injection
(DOI: 10.4126/FRL01-006409589).

Case #4

Video 4a: At 48 hours after enzyme injection and administration of anesthetic, the manipulation
video illustrates the extension maneuvers needed for correction required for these 2 digits
(DOI: 10.4126/FRL01-006409591).


Case #5

Video 5a: Injection of the interconnecting fourth and fifth ray cords is seen using slightly increased diluent volume (DOI: 10.4126/FRL01-006409593).
Video 5b: Manipulation at 48 hours post-collagenase, following anesthetic administration
(DOI: 10.4126/FRL01-006409595).


Case #6










Case #7

Video 7a: This shows injection technique beginning with the ring finger because – although the
little was more of a bother to him – it was not possible to get to those cords with the ring in the
way (DOI: 10.4126/FRL01-006409597).


Video 7b: At 48 hours post-collagenase finger manipulation was performed after anesthetic
injection. Considerable pull was needed – as can be seen and heard – to achieve correction
(DOI: 10.4126/FRL01-006409599).


Case #8

Video 8a: This shows injection technique for rare inter-phalangeal cords in this little finger
(DOI: 10.4126/FRL01-006409601).
Video 8b: At 48 hours post-collagenase, finger manipulation was performed after anesthetic
injection (DOI: 10.4126/FRL01-006409603).



References
[1] Xiaflex® (collagenase clostridium histolyticum) [prescribing information]. Malvern: Auxilium Pharmaceuticals Inc.; 2013.[2] European Medicines Agency. Assessment report: Xiapex. [cited 2016 Jul 12]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_asses...
[3] Desai SS, Hentz VR. Collagenase clostridium histolyticum for Dupuytren's contracture. Expert Opin Biol Ther. 2010;10(9):1395-404. DOI: 10.1517/14712598.2010.510509
[4] Auxilium Pharmaceuticals Inc. Briefing document for collagenase clostridium histolyticum (AA4500) in the treatment of advanced Dupuytren's disease. Available from: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMateria...
[5] Rydevik B, Brown MD, Ehira T, Nordborg C. Effects of collagenase on nerve tissue. An experimental study on acute and long-term effects in rabbits. Spine (Phila Pa 1976). 1985;10(6):562-6. DOI: 10.1097/00007632-198507000-00010
[6] Rydevik B, Ehira T, Linder L, Olmarker K, Romanus M, Branemark PI. Microvascular response to locally injected collagenase. An experimental investigation in hamsters and rabbits. Scand J Plast Reconstr Surg Hand Surg. 1989;23(1):17-21. DOI: 10.3109/02844318909067503
[7] Thomas A, Bayat A. The emerging role of Clostridium histolyticum collagenase in the treatment of Dupuytren disease. Ther Clin Risk Manage. 2010;6:557-72. DOI: 10.2147/TCRM.S8591
[8] Eckhard U, Schonauer E, Nuss D, Brandstetter H. Structure of collagenase G reveals a chew-and-digest mechanism of bacterial collagenolysis. Nat Struct Mol Biol. 2011;18(10):1109-14. DOI: 10.1038/nsmb.2127
[9] Kono T. Purification and partial characterization of collagenolytic enzymes from Clostridium histolyticum. Biochemistry. 1968;7(3):1106-14. DOI: 10.1021/bi00843a031
[10] Badalamente MA, Hurst LC. Enzyme injection as a nonoperative treatment for Dupuytren's Disease. Drug Deliv. 1996;3:35-40. DOI: 10.1021/bi00843a031
[11] Hueston JT. The table top test. The Hand. 1982;14(1):100-3. DOI: 10.1016/S0072-968X(82)80053-3
[12] Badalamente MA, Hurst LC. Enzyme injection as nonsurgical treatment of Dupuytren's disease. J Hand Surg Am. 2000;25(4):629-36. DOI: 10.1053/jhsu.2000.6918
[13] Badalamente MA, Hurst LC, Hentz VR. Collagen as a clinical target: nonoperative treatment of Dupuytren's disease. J Hand Surg Am. 2002;27(5):788-98. DOI: 10.1053/jhsu.2002.35299
[14] Hurst LC, Badalamente MA, Hentz VR, Hotchkiss RN, Kaplan FT, Meals RA, Smith TM, Rodzvilla J; CORD I Study Group. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009 Sep 3;361(10):968-79. DOI: 10.1056/NEJMoa0810866
[15] Gilpin D, Coleman S, Hall S, Houston A, Karrasch J, Jones N. Injectable collagenase clostridium histolyticum: a new nonsurgical treatment for Dupuytren's disease. J Hand Surg Am. 2010;35(12):2027-38. DOI: 10.1016/j.jhsa.2010.08.007
[16] Witthaut J, Jones G, Skrepnik N, Kushner H, Houston A, Lindau TR. Efficacy and safety of collagenase clostridium histolyticum, a nonsurgical treatment for adults with Dupuytren's contracture: short-term results from two open-label studies, in the US (JOINT I) and Australia and Europe (JOINT II). J Hand Surg Am. 2013;38(1):2-11. DOI: 10.1016/j.jhsa.2012.10.008
[17] Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007;32(6):767-74. DOI: 10.1016/j.jhsa.2007.04.002
[18] Zhang P, Qin L. Injectable collagenase clostridium histolyticum for Dupuytren's contracture [letters to editor and authors' reply]. N Engl J Med. 2009;361(26):2578-80. DOI: 10.1056/NEJMc0909497
[19] Witthaut J, Bushmakin AG, Gerber RA, Cappelleri JC, Le Graverand-Gastineau MP. Determining clinically important changes in range of motion in patients with Dupuytren's Contracture: secondary analysis of the randomized, double-blind, placebo-controlled CORD I study. Clin Drug Invest. 2011;31(11):791-8. DOI: 10.1007/BF03256918
[20] Zhang AY, Curtin CM, Hentz VR. Flexor tendon rupture after collagenase injection for Dupuytren contracture: case report. J Hand Surg Am. 2011;36(8):1323-5. DOI: 10.1016/j.jhsa.2011.05.016
[21] Peimer CA, Blazar P, Coleman S, Kaplan FT, Smith T, Tursi JP, Cohen B, Kaufman GJ, Lindau T. Dupuytren contracture recurrence following treatment with collagenase clostridium histolyticum (CORDLESS study): 3-year data. J Hand Surg Am. 2013 Jan;38(1):12-22. DOI: 10.1016/j.jhsa.2012.09.028
[22] Raven RB 3rd, Kushner H, Nguyen D, Naam N, Curtin C. Analysis of efficacy and safety of treatment with collagenase Clostridium histolyticum among subgroups of patients with Dupuytren contracture. Ann Plast Surg. 2014 Sep;73(3):286-90. DOI: 10.1097/SAP.0b013e31827ae9d0
[23] Coleman S, Gilpin D, Tursi J, Kaufman G, Jones N, Cohen B. Multiple concurrent collagenase clostridium histolyticum injections to Dupuytren's cords: an exploratory study. BMC Musculoskelet Disord. 2012;13:61. DOI: 10.1186/1471-2474-13-61
[24] Coleman S, Gilpin D, Kaplan FT, Houston A, Kaufman GJ, Cohen BM, Jones N, Tursi JP. Efficacy and safety of concurrent collagenase clostridium histolyticum injections for multiple Dupuytren contractures. J Hand Surg Am. 2014 Jan;39(1):57-64. DOI: 10.1016/j.jhsa.2013.10.002
[25] Bainbridge C, Gerber RA, Szczypa PP, Smith T, Kushner H, Cohen B, Hellio Le Graverand-Gastineau MP. Efficacy of collagenase in patients who did and did not have previous hand surgery for Dupuytren's contracture. J Plast Surg Hand Surg. 2012 Sep;46(3-4):177-83. DOI: 10.3109/2000656X.2012.683795
[26] Skirven TM, Bachoura A, Jacoby SM, Culp RW, Osterman AL. The effect of a therapy protocol for increasing correction of severely contracted proximal interphalangeal joints caused by Dupuytren disease and treated with collagenase injection. J Hand Surg Am. 2013;38(4):684-9. DOI: 10.1016/j.jhsa.2013.01.038
[27] Hotchkiss RN, Coleman SG, Smith T, Tursi JP, Kaufman GJ. Recurrence of Dupuytren's contracture after nonsurgical treatment with collagenase clostridium histolyticum: summary of 4-year CORDLESS data. J Hand Surg Am. 2013;38(10 suppl):e53-e54.
[28] Watt AJ, Curtain CM, Hentz VR. Collagenase injection as nonsurgical treatment of Dupuytren's disease: 8-year follow-up. J Hand Surg Am. 2010;35(4):534-9.
[29] Peimer CA, McGoldrick CA, Fiore GJ. Nonsurgical treatment of Dupuytren's contracture: 1-year US post-marketing safety data for collagenase clostridium histolyticum. Hand. 2012;7:143-6. DOI: 10.1007/s11552-012-9407-3
[30] Taylor AJ, Mandel D, Britton EN, Frazier JL, Kaufman G, Tursi J. Design and construction of a decision tree for treatment of Dupuytren's contracture. 67th Annual Meeting of the American Society for Surgery of the Hand; 2012 Sep 6-8; Chicago (US).



