Rare cases of urogenital tuberculosis and atypical mycobacterial urogenital infection
Svetlana Dubrovina 2
Denis Kholtobin 3
Victor Khomyakov 4
Mete Çek 5
1 Novosibirsk Research TB Institute, Novosibirsk State Medical University, Novosibirsk, Russland
2 Obstetrics and Gynaecology , Rostov Medical State University, Rostov-on-Don, Russland
3 Urology, Novosibirsk TB reseach institute, Novosibirsk, Russland
4 Novosibirsk Research TB Institute, Novosibirsk, Russian Federation
5 Urology, Trakya University, School of Medicine, Edirne, Türkei
Abstract
Tuberculosis is a multisystem disease with myriad presentations and manifestations; it can affect any organ or tissue, excluding only hair and nails. Doctors who are not familiar with extra-pulmonary tuberculosis may not include this disease in their differential diagnostic work-up. The share of urogenital tuberculosis among all extrapulmonary forms gets up to 47%, and it is more often revealed in developing countries.
1 Introduction
World Health Organization (WHO) defines tuberculosis (TB) as a global problem, however, mostly pulmonary TB (PTB) falls under the lights [1]. Urogenital TB (UGTB) doesn’t seem to be a primary concern for WHO, although UGTB is the third-second most common form of extrapulmonary TB. UGTB is an ancient disease and still presents many unsolved problems. Clinical features are flexible and variable; UGTB mimics numerous other diseases in which frequently delays appropriate diagnosis.
We used the following classification of UGTB [2], [3]:
- Kidney TB (KTB); KTB is divided into 4 stages, which depend on the level of destruction.
- Male genital tuberculosis (MGTB); which includes orchiepididymitis (mono- and bilateral), prostate TB (infiltrative or cavernous forms), TB of seminal vesicles and TB of penis
- Female genital tuberculosis (FGTB); when any female genital organ is infected with TB.
- Generalized UGTB when both kidneys and genitals are involved.
- Urinary tract tuberculosis (UTB) – is always secondary to KTB, includes TB of ureter, bladder TB of 1–4 grades, urethral TB. Complications of KTB/UTB: strictures, fistula, renal failure, arterial hypertension.
- Female genital tuberculosis.
- Generalized urogenital tuberculosis – simultaneous lesion of urinary organs and genitals; is always considered as complicated.
UGTB is an embodiment of contradictions – from terms and classification till therapy and management. Nevertheless, we have to overcome this quagmire for best understanding this eternal enigmatic and potentially fatal dangerous disease.
The purpose of this study was to discuss the difficulty of timely diagnosis of UGTB because of non-specific clinical picture, atypical course, the wont to hide under the mask of another disease.
2 Material and methods
For literature review we have searched MEDLINE/PubMed with the key words “urogenital tuberculosis”, “rare”, “unusual”. The search for “Urogenital tuberculosis” revealed 7,087 items, “urogenital tuberculosis rare” – 235 items and “urogenital tuberculosis unusual” – 16 items only. Actually most of these issues did not describe exactly rare and unusual cases of urogenital tuberculosis; we selected really unusual and rare cases. Finally, we analyzed the WHO report of 2016, and 57 scientific articles dedicated to unusual features of UGTB.
3 Results
3.1 Urogenital involvement in pulmonary TB patients
Urogenital involvement occurring synchronously with pulmonary tuberculosis (TB), which is frequent in patients with disseminated tuberculosis, may be puzzling. Generalized TB may manifest first with urogenital tuberculosis (UGTB). This scenario was described by Colbert et al. in their case report [4]. The patient presented with vomiting and renal colic. Imaging studies showed nodules throughout the lungs, retroperitoneum, abdominal viscera, and kidneys. Unilateral hydronephrosis was found on renal imaging.
Vulvar TB in a patient with a long history of pulmonary TB was diagnosed as sexually transmitted disease [5]. However, localized papulonecrotic tuberculid of the vulva was diagnosed timely in a 26-year-old Indian woman with lymphatic and pulmonary TB, thanks to a high index of suspicion [6].
3.2 Urogenital TB and cancer
Differential diagnosis of UGTB is very challenging, urogenital carcinoma being one of the most frequent misleading diagnosis. Isolated tuberculous epididymitis (ITE), defined as tuberculous epididymitis without clinical evidence of either renal or prostate involvement, is a rare entity among various clinical presentations of UGTB. Kho and Chan [7] reported a 20-year-old man who presented with a slow-growing painless scrotal mass for 2 months, with the initial workup suspicious for a right para-testicular tumor. Surgical resection of the mass was therefore scheduled. However, severe pain and redness over the patient's right hemi-scrotum were noted on the day of surgery. A repeat scrotal ultrasound revealed findings suggesting a chronic inflammatory process rather than a malignancy. Frozen section of the lesion confirmed the ultrasonographic findings, and the pathology established the diagnosis of ITE [7].
Isolated tuberculous epididymo-orchitis may closely mimic testicular tumour, particularly in patients with no history of systemic TB. A 44-year old man presented with 4 months’ history of left scrotal mass and underwent left orchidectomy following a preliminary diagnosis of testicular tumour. Histopathology revealed testicular tuberculosis [8]. TB orchiepididymitis, in another case was also preliminary misdiagnosed as scrotal tumor [9]. One more patient presented with a scrotal mass in 5 months after the prostate biopsy and was estimated as tumor and managed with unilateral simple orchiepidymectomy. Histopathology revealed TB [10].
Androulaki et al. [11] reported the case of an inflammatory pseudotumor associated with Mycobacterium tuberculosis (Mtb) infection, which was initially mistaken for a renal malignancy both in clinical and radiological settings.
Bouchikhi et al. [12] reported a patient presenting with left back pain associated with urinary frequency and a few macroscopic episodes of hematuria for the past six months. The helical computed tomography revealed a left hydronephrosis and hydroureter secondary to focal wall thickening of the left lumbar ureter. On this basis, authors diagnosed a ureteral tumor. However, a clinical examination showed irritative voiding symptoms as well as epididymitis associated with prostate infection suggesting Mtb assessment of the patient's urine of which the results proved strongly positive [12].
Female genital tuberculosis (FGTB) as well may be a reason for incorrect diagnosis of cancer. Sabita et al. [13] reported a rare case of isolated cervical TB which mimicked carcinoma of the cervix. A 24-year-old woman presented with secondary amenorrhea and post coital bleeding which were present for one year. Vaginal examination revealed a friable cervix which bled with contact. Though the clinical history and the examination findings were suggestive of a cervical malignancy, the histopathological examination revealed a granulomatous TB inflammation [13].
Jaiprakash et al. [14] emphasized that in countries like India, where carcinoma of cervix is very common, cervical TB may easily be mistaken clinically for malignancy. They reported a case of tuberculosis cervicitis (secondary to pulmonary tuberculosis) in a post-menopausal woman, who presented with the complaint of vaginal discharge for a short duration. Vaginal examination showed an ulcerated lesion over anterior the lip of cervix, clinically suggestive of malignancy. However, a Papanicolaou-smear showed features suggestive of TB which was confirmed by biopsy [14].
Massive uterovaginal prolapse with cervical lesion mimicked cervical carcinoma in the case described by Pei Shan Lim et al. [15], and surgery was performed, after histopathology confirmed TB. Vulvar tuberculosis in one case was diagnosed as vulvar carcinoma, and the patient underwent radical surgery, whereupon TB was found by histological investigation [16].
A 61-year-old postmenopausal woman who had undergone surgery and treated with adjuvant chemotherapy for infiltrating ductal carcinoma of the breast five years ago, presented with bloody vaginal discharge, fatigue, weight loss, and low grade fevers at night for two months. Histological examination of the endometrium, done based on the suspicion of a second primary cancer due to the tamoxifen therapy, revealed a granulomatous reaction, Mtb was found by GeneXpert system [17].
3.3 Urolithiasis as a mask and co-morbidity of UGTB
The same clinical features as well as laboratory and X-ray findings in urolithiasis and UGTB may conduce to misdiagnosis these diseases. Wong et al. [18] described a case of UGTB masquerading as a ureteral calculus. Gupta et al. [19] had a patient, who presented with bilateral urolithiasis and features of renal failure; he underwent left nephrectomy after thorough investigations. The biopsy revealed features of KTB. Later the patient underwent right ureteroscopic lithotripsy. Prakash et al. [20] have found confusing picture of extensive renal and ureteral calcification due to TB.
3.4 Bladder tuberculosis
Bladder TB is rather often complication of KTB, but its manifestation may be unusual and misguiding. Kumar et al. [21] reported 2 cases of a TB cavity behind the bladder and prostate which initially eluded diagnosis, and were confirmed only after surgery. Typical for bladder TB situation was reported by Kaneko et al. [22] (2008). A 24-year-old man experienced gross hematuria and dysuria several times a year from the age of 19, presenting to the Urological Department for the first time at age 21, when he was given standard antibiotic treatment for acute cystitis. Although urinary symptoms persisted, he failed to attend for follow-up. He attended another clinic at the age of 24 with increased urinary frequency. Transrectal ultrasonography revealed thickening of the bladder wall, concavity of the right bladder neck, and nodular changes extending from the left bladder neck to the left bladder wall, and Mtb was detected in the urine [22]. For a long time, bladder TB was overlooked – till it became complicated form grade 4.
Bladder TB grade 4 is unsuitable for conservative therapy; cystectomy with following urinary diversion urinary diversion is indicated. There is a risk of development a cancer of neobladder. Lopes et al. [23] presented a case of a 67-year-old patient with a history of augmentation ileocystoplasty 31 years ago because of UGTB. Radiological investigations performed due to asymptomatic microscopic hematuria revealed three contrast-enhancing polyps within the neobladder. The patient underwent enterocystoprostatectomy and histopathological examination of the neobladder revealed mucinous adenocarcinoma in all three polyps, together with a prostatic adenocarcinoma Gleason 7 (3+4) [23].
Spontaneous bladder perforation secondary to TB is very rare, and the diagnosis is often missed. Confirmation of TB via culture takes a long time and starting empirical treatment for TB is necessary. Kong et al. [24] reported a young woman who presented with clinical features of a perforated appendix and was only diagnosed with bladder perforation during laparotomy. She also had distal right ureteral stricture and left infundibular stenosis. The provisional diagnosis of TB was attained via typical histopathological features and a positive Mantoux test. Kumar et al. [25] and Vallejo et al. [26] also described spontaneous bladder rupture secondary to UGTB.
3.5 TB of urethra
Bouchikhi et al. [27] reported an incredible case of UGTB in a man revealed by urethral narrowing and multiple urethro-scrotal fistulas. The patient presented with dysuria, purulent discharge and a meatic penoscrotal fistula. A retrograde and voiding urethrocystography was performed and revealed an extended narrowing of the whole anterior urethra associated with multiple fistulous portions toward the scrotum and perineum. His condition was estimated as nonspecific sclero-inflammatory urethral stricture with complicating fistulas, and patient underwent an urethroplasty. The wound healing was delayed and associated with the persistence of fistulas extending into the corpus cavernosum with purulent discharge. Only now TB was suspected; multiple biopsies were then performed on the periurethral tissue and fistula tracts, and the histological examination confirmed the diagnosis [27]. We suppose in fact in this case there was un-revealed KTB, as TB of urogenital tract is a complication of KTB.
3.6 TB of epididymitis
Rakototiana et al. [28] had met difficulties in diagnosis of isolated testicular tuberculosis in 2 children. The clinical features had no specificity: one case of hydrocele and 1 case of acute scrotal inflammation. Surgical exploration showed testicular nodules in both cases. Only histological examination provided the definitive diagnosis.
A trauma may provoke the exacerbation of the latent TB. The persistent hypertrophy of the right epididymis in young men had been regarded as a sequela of a recent trauma of the scrotum. The diagnosis of tuberculosis was confirmed by epididymal biopsy, by intravenous urography which revealed a cavity in a left superior calix and above all by the presence of Mtb at bacteriological urine examination [29].
3.7 TB of penis
Surprisingly many authors reported on TB of glans penis – and not only as a complication of BCG-therapy for superficial bladder cancer and bladder carcinoma [30].
Cutaneous penile TB in an HIV-positive man masquerading a sexually transmitted infection was confirmed by positive cultures [31]. Toledo-Pastrana et al. [32] reported the case of a patient with ulcerous penile TB, presumably acquired through sexual intercourse. Kar and Kar [33] have found primary TB of penis in a 31 years old male patient who presented with some ulcerated lesions on the glans penis. Diagnosis was established as primary tuberculosis of glans penis, confirmed by biopsy and supported by a strongly positive Mantoux test and positive TB-PCR. There was no co-existing tuberculous infection elsewhere.
Also Sah et al. [34]. (1999) revealed a 60-year-old man presenting with multiple superficial ulcers on the glans penis. Histopathology, a positive tuberculin test result, and therapeutic response to antituberculous therapy confirmed the diagnosis of penile TB. Examination was otherwise normal except for a solitary enlarged reactive lymph node on the right side. And again there was no evidence of coexistent TB infection elsewhere.
Baskin and Mee [35] reported a case of penis TB that presented as a subcutaneous nodule without superficial ulceration as well as Yonemura et al. [36] who have experienced a case of penis TB that appeared as a scab on nodule. A 56-year-old man presented with a 4-month history of a painless subcutaneous nodule at the glans penis. Pathological findings of the nodule showed granulomatous inflammation. Tuberculin tests were strongly positive, but Mtb could not be detected. Savu et al. [37] (2012) presented a case of penile tuberculosis with a bulky penoscrotal formation treated previously for the suspicion of Fournier gangrene.
Karthikeyan et al. [38] described “Water can” penis caused by TB, which was misdiagnosed for a long time. Nakamura et al. [39] discovered 37 cases of TB of penis in Japan in 10 years (between 1978 and 1987).
3.8 Prostate TB
Otherwise isolated prostate TB is more often localization of UGTB. As an example a historical case of a 65-year-old man was described. The patient presented with symptoms of frequency, dysuria and hesitancy, and 10 kg weight loss in the last 6 months, without pulmonary symptoms and negative ELISA test for HIV. Digital rectal examination (DRE) revealed a high volume, irregular and hard prostatic gland. Ultrasound investigation showed a prostatic volume of 39 cm3, without signs of malignancy. Biopsy of the prostatic gland showed multiple granulomas and the Ziehl-Nelsen staining was positive for Mtb [40].
Another case is a 64-year-old man who presented with an obstructive syndrome of the lower urinary tract. After clinical and laboratory examination, prostate cancer was highly suspected. Transrectal biopsy was performed and histological examination showed tuberculous lesions [41].
3.9 Fatal cases of UGTB
Renal TB is difficult to diagnose, because many patients present themselves with lower urinary symptoms which are typical for bacterial cystitis. Delayed diagnosis may have grave consequences – even fatal. The case of a young woman with renal TB was reported by Daher et al. (2007). The patient was admitted with complaints of adynamia, anorexia, fever, weight loss, dysuria and generalized edema for 10 months. At physical examination she was febrile (39°C), and her abdomen had increased volume and was painful at palpation. Laboratorial tests showed azotemia, leukocytosis, leukocyturia and proteinuria. She was also oliguric. Abdominal echography showed thick and contracted bladder walls and heterogeneous liquid collection in the left pelvic region. Two laparotomies were performed, in which an abscess in the pelvic region was found. Anti-TB treatment with rifampin, isoniazid and pyrazinamide was started. During the follow-up, the urine culture was found to be positive for Mtb. The complex therapy was unsuccessful, and hemodialysis was then started. The computed tomography showed signs of chronic nephropathy, dilated calyces and thinning of renal cortex in both kidneys and severe dilatation of the ureter. The patient developed neurologic symptoms, suggesting TB meningoencephalitis, and died despite of support measures adopted [42].
Dadhwal et al. [43] reported a rare case of TB flare in a 28-year-old nulliparous woman following endometrial aspiration, which drained 30 ml pus. Following this, she developed high-grade fever with pain abdomen, guarding and rigidity. PCR was positive for mycobacterium and histopathology showed necrotizing granulomatous endometritis. She also showed features of FGTB and chronic TB meningitis.
3.10 Tuberculosis of the renal artery as a cause of renovascular arterial hypertension
Bouziane et al. [44] have reported tuberculosis of the renal artery. A 17-year-old patient presenting with renovascular arterial hypertension, was revealed by the ultrasonography, when an occlusion of the right renal artery as well as pararenal and mesenteric polyadenopathy were found. Authors supposed TB etiology of both processes and anti-TB treatment had been carried out. In one month the right renal artery was revascularized with a right iliorenal bypass using reversed internal saphenous vein. The patient was operated with an 18-month follow-up. Arterial pressure was normal without antihypertensive treatment. This case is interesting, but diagnosis was confirmed by good efficiency of anti-TB therapy, not by histology nor bacteriology.
3.11 Granulomatous interstitial nephritis due to tuberculosis
Granulomatous interstitial nephritis (GIN) is an uncommon form of acute interstitial nephritis. Sampathkumar et al. [45] reported the case of a young male who presented with a rapidly progressing renal failure and massive proteinuria. A renal biopsy revealed GIN, and Mtb DNA was found in the biopsy specimen by PCR. The patient was started on anti-TB therapy and steroids besides 11 sessions of hemodialysis.
3.12 Tuberculosis of the uterine cervix
Patients with TB of the uterine cervix were observed by Yang et al., Giacopino et al., Lamba et al. [46], [47], [48]. In our practice as well there were 5 patients with uterine cervix TB, and three of them had sexual partner with prostate TB, and two denied any contact with TB infection.
Singh et al. [49] described two cases of tuberculous cervicitis with variable clinical presentation. In one case, a young woman presented with primary infertility and secondary amenorrhoea. The other is a perimenopausal woman with irregular vaginal bleeding and postcoital blood-stained discharge. The diagnosis was confirmed on histopathological examination of the endocervical curettings and a cervical biopsy.
3.13 Vulva and vagina TB
A 60-year-old woman was admitted to the Department of Obstetrics and Gynecology due to chronic extensive painful genital ulcer. She was treated by antiviral and antifungal regimens but the ulcer persisted. Tissue biopsy was performed then, and acid fast bacilli were found [50].
Nemati et al. [51] also observed a woman that developed vaginal tuberculosis one year after receiving a kidney transplant from a living donor. Her complaints included abdominal pain, fever, and weight loss. Furthermore, her tuberculin skin test was negative.
Sharma et al. [52] reported a case of tubercular vulvar ulcer in a sexually inactive pubertal girl. She had a close contact with active tuberculosis, positive tuberculin skin test, and chronic granulomatous inflammation on vulvar biopsy.
Tiwari et al. [53] reported a case of hypertrophic vulvar tuberculosis of primary origin in a 26-year-old female patient. The diagnosis was mainly based on histopathological examination.
3.14 Overlooked tubo-ovarian tuberculomas
A case of tubo-ovarian tuberculosis mimicking acute appendicitis was described by Akbulut et al. [54]. A 17-year-old woman presented with complaints of right lower quadrant abdominal pain, nausea, and vomiting. Her physical examination findings, ultrasonogram, and leukocyte count were consistent with acute appendicitis. A cystic mass (15 cm × 6 cm) was detected on the right tubo-ovarian structure by laparotomy. The mass was excised while the tubo-ovarian structures were preserved and the need for an appendectomy was avoided. No microbiological evaluation was performed. The histopathological examination of the cystic mass revealed a granuloma with central caseating necrosis surrounded by epithelioid histiocytes [54].
A similar case was presented by Ilmer et al. [55]. A 35-year-old human immunodeficiency virus seropositive woman complained of lower abdominal pain and fever of two days. She underwent surgery due to left adnexal mass suggesting pelvic inflammatory disease. The surgical situs showed four quadrant peritonitis provoked by a tubo-ovarian abscess on the left side. Histopathological evaluation identified a necrotic granulomatous salpingitis and Mtb was identified by PCR.
Exacerbation of latent genital tuberculosis during in vitro fertilisation and pregnancy was described by Huang et al. [56].
3.15 Congenital tuberculosis
The patient of Agrawal et al. [57] was less lucky. They described the case of a male preterm baby who had congenital miliary tuberculosis with multiple intestinal perforations because his mother had widespread destructive pulmonary tuberculosis.
Two cases of congenital TB were reported by Das et al. [58]. The first one was presented at 12 days of age. The mother had been symptomatic for TB in the first trimester but was not diagnosed until her infant developed symptoms. The infant̓s gastric aspirate was acid-fast bacilli (AFB) positive and Mtb-culture positive. PCR on the gastric specimen and mother's sputum demonstrated identical strains. The second baby was presented at 45 days of age and the gastric aspirate was both AFB- and culture-positive. The mother was asymptomatic and contact-tracing of the family failed to detect infection. However, FGTB was found in the mother’s endometrial biopsy [58].
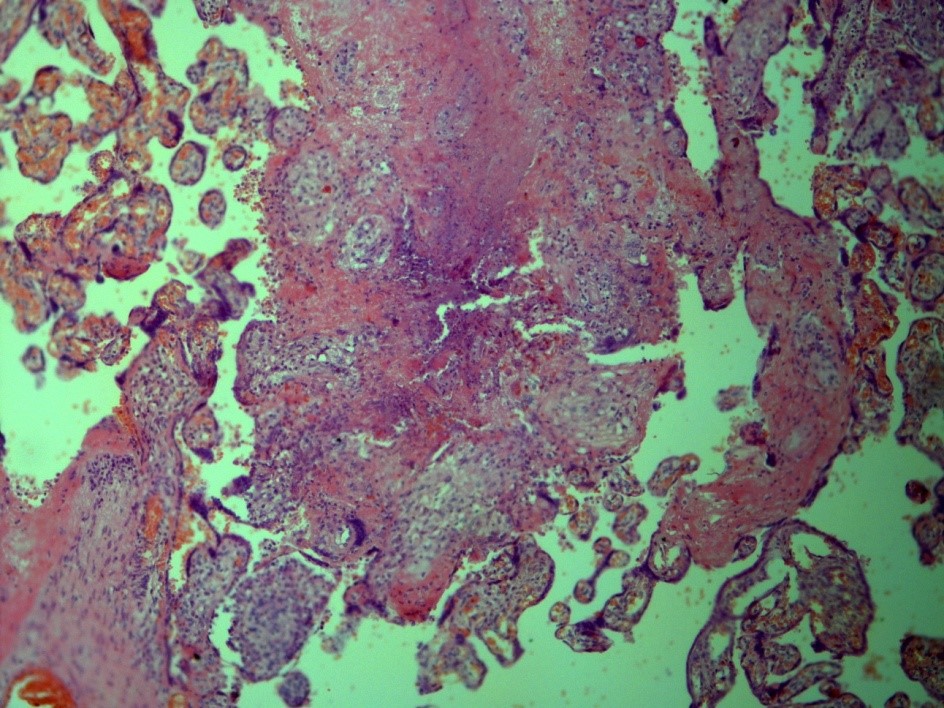
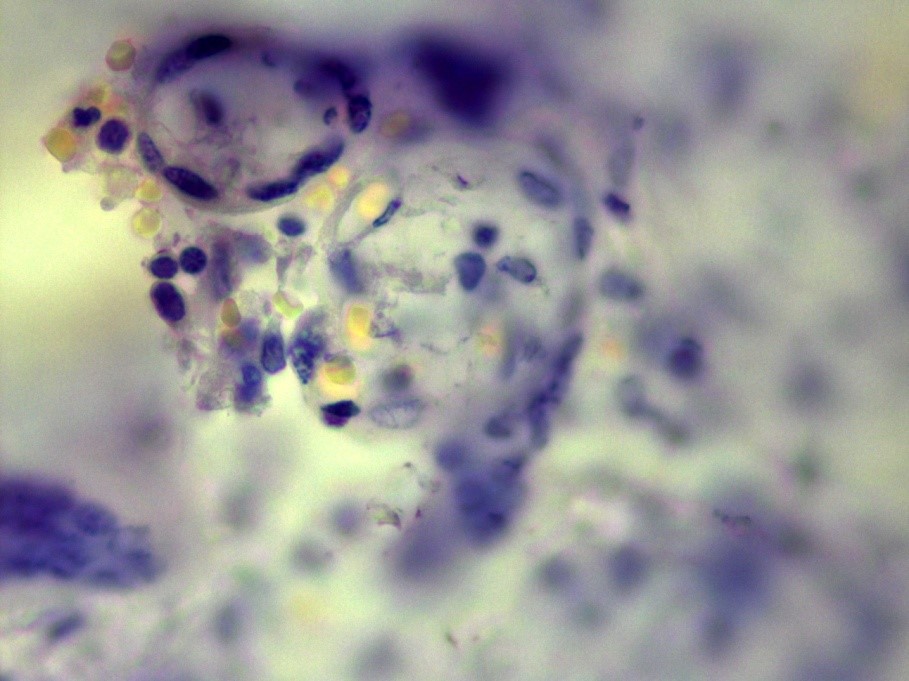
Our own case demonstrates an extremely rare case of TB of placenta in young woman, suffering from genital TB, which was overlooked before delivery. This woman had not known contact with TB infection, had no history of TB, had no complaints before pregnancy and had no special complaints in time of the pregnancy, excluding common ones for this condition. The delivery was in-time with a healthy full-term baby. In the Russian Federation the investigation of the placenta is a standard procedure, and it revealed TB inflammation (Figure 1) and Mtb in the placenta (Figure 2).
4 Conclusion
Actually UGTB is not a rare disease – but it is an often overlooked disease. The main reasons for delayed diagnostics are two: vague clinical features and a low index of suspicion. We cannot ignore UGTB – late diagnosis mandatory leads to loss of organ. UGTB is an infectious contagious disease, and it is one more reason for its early diagnosis. It is necessary to use all arsenals of bacteriology and histology to confirm UGTB.
References
[1] World Health Organization. Global tuberculosis report 2018. Geneva: World Health Organization; 2018. Available from: https://www.who.int/tb/publications/global_report/en/[2] Kulchavenya E, Naber K, Bjerklund Johansen TE- Urogenital tuberculosis: classification, diagnosis, and treatment. Eur Urol Suppl. 2016;15(4):112-21. DOI: 10.1016/j.eursup.2016.04.001
[3] Kulchavenya E. Urogenital tuberculosis. In: AAUS Guideline Development Group, editor. UAA-AAUS Guidelines for Urinary Tract Infections and Sexually Transmitted Diseases. 2016. Available from: http://www.aaus.info/mediawiki/index.php/Urogenital_tuberculosis
[4] Colbert G, Richey D, Schwartz JC. Widespread tuberculosis including renal involvement. Proc (Bayl Univ Med Cent). 2012 Jul;25(3):236-9. DOI: 10.1080/08998280.2012.11928836
[5] Nanjappa V, Suchismitha R, Devaraj HS, Shah MB, Anan A, Rahim SN. Vulval tuberculosis - an unusual presentation of disseminated tuberculosis. J Assoc Physicians India. 2012 Dec;60:49-52.
[6] Wong S, Rizvi H, Cerio R, O'Toole EA. An unusual case of vulval papulonecrotic tuberculid. Clin Exp Dermatol. 2011 Apr;36(3):277-80. DOI: 10.1111/j.1365-2230.2010.03925.x
[7] Kho VK, Chan PH. Isolated tuberculous epididymitis presenting as a painless scrotal tumor. J Chin Med Assoc. 2012 Jun;75(6):292-5. DOI: 10.1016/j.jcma.2012.04.014
[8] Badmos KB. Tuberculous epididymo-orchitis mimicking a testicular tumour: a case report. Afr Health Sci. 2012 Sep;12(3):395-7.
[9] Lakmichi MA, Kamaoui I, Eddafali B, Sellam AI, Dahami Z, Moudouni SM, Sarf I. An unusual presentation of primary male genital tuberculosis. Rev Urol. 2011;13(3):176-8.
[10] Yu-Hung Lai A, Lu SH, Yu HJ, Kuo YC, Huang CY. Tuberculous epididymitis presenting as huge scrotal tumor. Urology. 2009 May;73(5):1163.e5-7. DOI: 10.1016/j.urology.2008.04.015
[11] Androulaki A, Papathomas TG, Liapis G, Papaconstantinou I, Gazouli M, Goutas N, Bramis K, Papalambros A, Lazaris AC, Papalambros E. Inflammatory pseudotumor associated with Mycobacterium tuberculosis infection. Int J Infect Dis. 2008 Nov;12(6):607-10. DOI: 10.1016/j.ijid.2007.12.011
[12] Bouchikhi AA, Amiroune D, Tazi MF, Mellas S, Elammari JE, El Fassi MJ, Khallouk A, Farih MH. Isolated urethral tuberculosis in a middle-aged man: a case report. J Med Case Rep. 2013 Apr 8;7:97. DOI: 10.1186/1752-1947-7-97
[13] Sabita S, Sharmila V, Arun Babu T, Sinhasan SP, Darendra S. A Rare Case of Cervical Tuberculosis which Simulated Carcinoma of the Cervix. J Clin Diagn Res. 2013 Jun;7(6):1189-90. DOI: 10.7860/JCDR/2013/5460.3077
[14] Jaiprakash P, Pai K, Rao L. Diagnosis of tuberculous cervicitis by Papanicolaou-stained smear. Ann Saudi Med. 2013 Jan-Feb;33(1):76-8. DOI: 10.5144/0256-4947.2012.23.5.1115
[15] Lim PS, Atan IK, Naidu A. Genitourinary tuberculosis: an atypical clinical presentation. Case Rep Obstet Gynecol. 2012;2012:727146. DOI: 10.1155/2012/727146
[16] Mallya V, Yadav YK, Gupta K. Vulval tuberculosis masquerading as vulval carcinoma. J Postgrad Med. 2012 Oct-Dec;58(4):307-8. DOI: 10.4103/0022-3859.105463
[17] Neonakis I, Mantadakis E, Gitti Z, Mitrouska I, Manidakis LG, Maraki S, Samonis G. Genital tuberculosis in a tamoxifen-treated postmenopausal woman with breast cancer and bloody vaginal discharge. Ann Clin Microbiol Antimicrob. 2006 Sep;5:20. DOI: 10.1186/1476-0711-5-20
[18] Wong N, Hoag NA, Jones EC, Rowley A, McLoughlin MG, Paterson RF. Genitourinary tuberculosis masquerading as a ureteral calculus. Can Urol Assoc J. 2013 May-Jun;7(5-6):E363-6. DOI: 10.5489/cuaj.1219
[19] Gupta S, R S, Meitei KS, Singh SR. Primary genito-urinary tuberculosis with bilateral urolithiasis and renal failure-an unusual case. J Clin Diagn Res. 2013 May;7(5):927-9. DOI: 10.7860/JCDR/2013/5570.2979
[20] Prakash J, Goel A, Sankhwar S, Singh BP. Extensive renal and ureteral calcification due to tuberculosis: rare images for an uncommon condition. BMJ Case Rep. 2013 Feb 6;2013. pii: bcr2012008508. DOI: 10.1136/bcr-2012-008508
[21] Kumar A, Srivastava A, Mishra VK, Banerjee G. Tubercular cavity behind the prostate and bladder: an unusual presentation of genitourinary tuberculosis. J Urol. 1994 May;151(5):1351-2. DOI: 10.1016/S0022-5347(17)35250-3
[22] Kaneko T, Kudoh S, Matsushita N, Kashiwabara Y, Tamura T, Yoshida I, Nomura K. [Case of bladder tuberculosis with onset at the age of nineteen--treatment of urinary tract tuberculosis in accordance with the new Japanese Tuberculosis Treatment Guidelines]. Nippon Hinyokika Gakkai Zasshi. 2008 Jan;99(1):29-34. DOI: 10.5980/jpnjurol1989.99.29
[23] Lopes FA, Rolim N, Rodrigues T, Canhoto A. Intestinal adenocarcinoma in an augmented ileocystoplasty. BMJ Case Rep. 2013 Aug 1;2013. pii: bcr2013009499. DOI: 10.1136/bcr-2013-009499
[24] Kong CH, Ali SA, Singam P, Hong GE, Cheok LB, Zainuddin ZM. Spontaneous bladder perforation: a rare complication of tuberculosis. Int J Infect Dis. 2010 Sep;14 Suppl 3:e250-2. DOI: 10.1016/j.ijid.2009.10.006
[25] Kumar RV, Banerjee GK, Bhadauria RP, Ahlawat R. Spontaneous bladder perforation: an unusual management problem of tuberculous cystitis. Aust N Z J Surg. 1997 Jan;67(1):69-70. DOI: 10.1111/j.1445-2197.1997.tb01904.x
[26] Vallejo Gil C, Palacio EV, Reig Ruiz C, Raventos Busquets C, Morote Robles J, Soler Roselló A. [Spontaneous bladder rupture secondary to urinary tuberculosis]. Actas Urol Esp. 1994 Sep;18(8):829-32.
[27] Bouchikhi AA, Amiroune D, Tazi MF, Mellas S, Elammari JE, El Fassi MJ, Khallouk A, Farih MH. Pseudotumoral tuberculous ureteritis: a case report. J Med Case Rep. 2013 Feb 15;7:45. DOI: 10.1186/1752-1947-7-45
[28] Rakototiana AF, Hunald FA, Razafimanjato N, Ralahy MF, Rakoto-Ratsimba HN, Rantomalala HY. Tuberculose testiculaire isolée chez l'enfant. A propos de 2 cas malgaches [Isolated testicular tuberculosis in children. Report of 2 Malagasy cases]. Arch Pediatr. 2009 Feb;16(2):112-4. DOI: 10.1016/j.arcped.2008.11.017
[29] Michel P. Tuberculose urogénitale révélée par un traumatisme des bourses [Urogenital tuberculosis revealed by scrotal trauma]. Presse Med. 1990 Sep;19(31):1454-5.
[30] Chowdhury AR, Dey RK. Penile tuberculosis following intravesical Bacille Calmette-Guérin immunotherapy. Indian J Urol. 2013 Jan;29(1):64-6. DOI: 10.4103/0970-1591.109989
[31] Stockamp NW, Paul S, Sharma S, Libke RD, Boswell JS, Nassar NN. Cutaneous tuberculosis of the penis in an HIV-infected adult. Int J STD AIDS. 2013 Jan;24(1):57-8. DOI: 10.1258/ijsa.2012.012103
[32] Toledo-Pastrana T, Ferrándiz L, Pichardo AR, Muniaín Ezcurra MA, Camacho Martínez FM. Tuberculosis: an unusual cause of genital ulcer. Sex Transm Dis. 2012 Aug;39(8):643-4. DOI: 10.1097/OLQ.0b013e318251577b
[33] Kar JK, Kar M. Primary tuberculosis of the glans penis. J Assoc Physicians India. 2012 Aug;60:52-3.
[34] Sah SP, AshokRaj G, Joshi A. Primary tuberculosis of the glans penis. Australas J Dermatol. 1999 May;40(2):106-7. DOI: 10.1046/j.1440-0960.1999.00332.x
[35] Baskin LS, Mee S. Tuberculosis of the penis presenting as a subcutaneous nodule. J Urol. 1989 Jun;141(6):1430-1. DOI: 10.1016/S0022-5347(17)41336-X
[36] Yonemura S, Fujikawa S, Su JS, Ohnishi T, Arima K, Sugimura Y. Tuberculid of the penis with a scab on the nodule. Int J Urol. 2004 Oct;11(10):931-3. DOI: 10.1111/j.1442-2042.2004.00917.x
[37] Savu C, Surcel C, Mirvald C, Gîngu C, Hortopan M, Sinescu I. Atypical primary tuberculosis mimicking an advanced penile cancer. Can we rely on preoperative assessment? Rom J Morphol Embryol. 2012;53(4):1103-6.
[38] Karthikeyan K, Thappa DM, Shivaswamy KN. "Water can" penis caused by tuberculosis. Sex Transm Infect. 2004 Feb;80(1):75. DOI: 10.1136/sti.2003.007203
[39] Nakamura S, Aoki M, Nakayama K, Kanamori S, Onda S. Penis tuberculid (papulonecrotic tuberculid of the glans penis): treatment with a combination of rifampicin and an extract from tubercle bacilli (T.B. vaccine). J Dermatol. 1989 Apr;16(2):150-3. DOI: 10.1111/j.1346-8138.1989.tb01238.x
[40] López Barón E, Gómez-Arbeláez D, Díaz-Pérez JA. Tuberculosis prostática primaria. Presentación de un caso y revisión de la literatura [Primary prostatic tuberculosis. Case report and bibliographic review]. Arch Esp Urol. 2009 May;62(4):309-13.
[41] Rabesalama SS, Rakoto-Ratsimba HN, Rakototiana AF, Razafimahatratra R, Raherison RA, Rantomalala HY, Randrianjafisamindrakotroka NS. [Isolated prostate tuberculosis. Report of a case in Madagascar]. Prog Urol. 2010 Apr;20(4):314-6. DOI: 10.1016/j.purol.2009.06.004
[42] Daher Ede F, Silva Júnior GB, Damasceno RT, Santos GM, Corsino GA, Silva SL, Gutiérrez-Adrianzén OA. End-stage renal disease due to delayed diagnosis of renal tuberculosis: a fatal case report. Braz J Infect Dis. 2007 Feb;11(1):169-71. DOI: 10.1590/S1413-86702007000100036
[43] Dadhwal V, Gupta N, Bahadur A, Mittal S. Flare-up of genital tuberculosis following endometrial aspiration in a patient of generalized miliary tuberculosis. Arch Gynecol Obstet. 2009 Sep;280(3):503-4. DOI: 10.1007/s00404-009-1082-4
[44] Bouziane Z, Boukhabrine K, Lahlou Z, Benzirar A, el Mahi O, Lekehal B, Mesnaoui A, Bensaid Y. Tuberculosis of the renal artery: a rare cause of renovascular arterial hypertension. Ann Vasc Surg. 2009 Nov-Dec;23(6):786.e7-9. DOI: 10.1016/j.avsg.2008.02.022
[45] Sampathkumar K, Sooraj YS, Mahaldar AR, Ramakrishnan M, Rajappannair A, Nalumakkal SV, Erode E. Granulomatous interstitial nephritis due to tuberculosis-a rare presentation. Saudi J Kidney Dis Transpl. 2009 Sep;20(5):842-5.
[46] Yang CT, Lee YH, Hsu GJ. Tuberculosis of the uterine cervix. Taiwan J Obstet Gynecol. 2012 Sep;51(3):449-51. DOI: 10.1016/j.tjog.2012.07.026
[47] Giacopino D, Colavita D. T.B.C. isolata del collo dell'utero. Sulle difficoltà diagnostiche della lesione tubercolare della cervice uterina: presentazione di due casi [Isolated tuberculosis of the uterine cervix. On the diagnostic difficulties in tuberculous lesions of the uterine cervix: presentation of 2 cases]. Arch Ostet Ginecol. 1968 Jan-Feb;73(1):71-83.
[48] Lamba H, Byrne M, Goldin R, Jenkins C. Tuberculosis of the cervix: case presentation and a review of the literature. Sex Transm Infect. 2002 Feb;78(1):62-3. DOI: 10.1136/sti.78.1.62
[49] Singh S, Gupta V, Modi S, Rana P, Duhan A, Sen R. Tuberculosis of uterine cervix: a report of two cases with variable clinical presentation. Trop Doct. 2010 Apr;40(2):125-6. DOI: 10.1258/td.2009.090423
[50] Buppasiri P, Temtanakitpaisan T, Somboonporn W. Tuberculosis at vulva and vagina. J Med Assoc Thai. 2010 May;93(5):613-5.
[51] Nemati E, Taheri S, Nourbala MH, Einollahi B. Vaginal tuberculosis in an elderly kidney transplant recipient. Saudi J Kidney Dis Transpl. 2009 May;20(3):465-7.
[52] Sharma C, Shekhar S, Sharma V, Sharma M, Aggarwal T. Paucibacillary tubercular vulval ulcer in a sexually inactive pubertal girl: role of therapeutic trial. J Pediatr Adolesc Gynecol. 2012 Dec;25(6):e123-4. DOI: 10.1016/j.jpag.2012.07.005
[53] Tiwari P, Pal DK, Moulik D, Choudhury MK. Hypertrophic tuberculosis of vulva--a rare presentation of tuberculosis. Indian J Tuberc. 2010 Apr;57(2):95-7.
[54] Akbulut S, Arikanoglu Z, Basbug M. Tubercular tubo-ovarian cystic mass mimicking acute appendicitis: a case report. J Med Case Rep. 2011 Aug 10;5:363. DOI: 10.1186/1752-1947-5-363
[55] Ilmer M, Bergauer F, Friese K, Mylonas I. Genital tuberculosis as the cause of tuboovarian abscess in an immunosuppressed patient. Infect Dis Obstet Gynecol. 2009;2009:745060. DOI: 10.1155/2009/745060
[56] Huang HJ, Xiang DR, Sheng JF. Exacerbation of latent genital tuberculosis during in vitro fertilisation and pregnancy. Int J Tuberc Lung Dis. 2009 Jul;13(7):921.
[57] Agrawal RL, Rehman H. Congenital miliary tuberculosis with intestinal perforations. Tuber Lung Dis. 1995 Oct;76(5):468-9. DOI: 10.1016/0962-8479(95)90017-9
[58] Das A, Arora J, Rana T, Porwal C, Kaushik A, Gaur G, Thukral A, Verma S, Kabra SK, Singh UB. Congenital tuberculosis: the value of laboratory investigations in diagnosis. Ann Trop Paediatr. 2008 Jun;28(2):137-41. DOI: 10.1179/146532808X302161




