Strategy-based evaluation of a formative simulation test assessing professionally relevant competences of undergraduate medical students
Sarah Prediger 1Julia Gärtner 1
Lea Jebram 1
Sigrid Harendza 1
1 Universitätsklinikum Hamburg-Eppendorf, III. Medizinische Klinik, Hamburg, Germany
Abstract
Objectives: A strategy-based evaluation of new teaching or examination formats is recommended in order to check their suitability before a possible integration into a medical curriculum. The aim of the project was to evaluate an established formative competence- and simulation-based examination format for medical students in a standardized way.
Project description: In a realistic simulation of a first working day in hospital, medical students at the end of their studies were given the opportunity to test their medical competences and to develop them further on the basis of self-assessment and feedback. In the years 2020 to 2023, a total of 879 students participated. This included 707 students in their final year (PJ) and 172 students before their PJ. The simulation format was evaluated in a standardized manner based on the Stanford criteria for evaluating clinical teaching. The free text comments were analyzed by content using MAXQDA.
Results: The quality of the training, the practical learning content and aspects of the individual training phases are the most important areas of the student evaluation. The learning atmosphere, the leadership and the assessments and feedback received are described positively. There are also clear indications that the simulation format promotes understanding and retention and supports self-directed learning well. Overall, participants gave the teaching format an average school grade of 1.26±.45. Some evaluation results have already been implemented in the adaptation of the simulation.
Conclusion: The integration of the simulation format into medical curricula can be recommended on the basis of this evaluation. Further development of the format is also possible.
Keywords
evaluation, feedback, formative assessment, communication, competences, simulation
1. Introduction
Responsible medical work and action is expected of graduates of human medicine studies upon licensure resp. from the first day of further medical training. This requires the acquisition of competences that are mapped in the National Competence-Based Learning Objectives Catalog for Medicine (NKLM) [https://nklm.de/zend/menu] and should be acquired during the six-year studies. Since competence is the ability to act responsibly and appropriately in a given context by integrating complex knowledge, skills and attitudes [1], [2], simulation formats are suitable for learning and testing competences in order to demonstrate responsible and competent medical action. Before new teaching or examination formats are integrated into a curriculum, it is advisable to first establish them as voluntary offers and evaluate their suitability.
The Federal Ministry of Health’s draft bill, which also provides for “the reorganization of examinations and the introduction of new, modern examination formats” ([3], p.1), is intended, among other things, to better depict communication with patients in history taking and the medical management of patients ([3], p.14). For the final year (PJ), it is also planned to complete a minimum number of structured patient presentations ([3], p.35f.). Furthermore, universities are to be obliged to offer courses that prepare students for the third stage of the medical examination [3].
The overarching aim of the project was, therefore, to evaluate an established format [4] for its suitability of integration into the curriculum, which supports medical students in the acquisition and self-reflection of medical skills based on feedback. To this end, students were given the opportunity to test their medical competences in a realistic simulation of a first working day in hospital [4] and to develop them further on the basis of self-assessment and feedback. The evaluation serves to improve teaching and is, therefore, an inherent part of it [5], whereby teaching quality is a multidimensional construct. In terms of methodology and practice, the evaluation strategy essentially followed the recommendations outlined in the position paper of the GMA committee “teaching evaluation” [6].
2. Project description
In the present project, a strategy-based content evaluation based on the Stanford criteria for the evaluation of clinical teaching [7] was carried out for a formative competence-based simulation assessment of a telemedical first working day in hospital [8]. From 2020 to 2023, a total of 879 students took part in the formative simulation assessment. This included 707 students in the PJ and 172 students before the PJ (semesters 6 to 12). In addition, 303 students took part in the simulation format repeatedly. The participants were on average 26.8±3.6 years old and 66.6% were female. Participation was voluntary and places were allocated according to the order of registrations received.
2.1. Formative simulation assessment
The formative simulation assessment of a first working day in hospital is based on a validated simulation format [4], which has been carried out as a telemedical format since 2020 [8] and comprises three basic phases:
- consultation hour,
- case preparation,
- case presentation and discussion round with an attending physician.
The conversion of the format from face-to-face to digital implementation had no impact on the basic process. The structure of all phases is identical. The patient interviews and group discussions now take place digitally. The only differences are that the students participate from home, i.e. they are physically “alone”, and the aspect of telemedical care for patients has now become part of the simulation (see figure 1 [Fig. 1]).
Figure 1: Procedure of the simulation format with human resources
The simulation was established on the basis of the ten most important, consented competence facets for beginning residents [9]. Some of the competence facets represent general learning objectives across the simulation, while others include specific learning objectives in the three basic phases (see table 1 [Tab. 1]). The other practical learning objectives of the simulation format are practicing focused history taking and case presentation as well as differential diagnostic thinking.
Table 1: Learning objectives in different competence areas according to simulation phases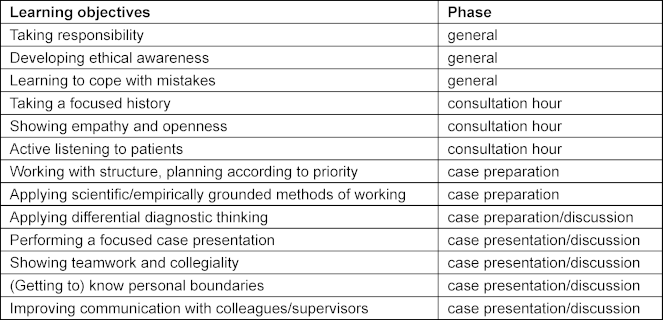
An assessment tool for medical communication and interpersonal skills (ComCare) was validated for the consultation hour [10], which was used by the simulated patients to provide feedback to the students. A digital documentation possibility was created for the management phase. Participants were able to view various patient findings for the handover discussion or case presentation. This was followed by a digital case discussion in groups of four, each with an attending physician, so that – from the students’ perspective – all four clinical pictures of the patients they had seen during the consultation hour were discussed.
The formative simulation assessment offered in the sense of deliberate practice [11] is advertised to the target group of students with the opportunity to test their own competences. Reference is made to the learning gain in terms of the acquisition of “adaptive expertise” [12]. For the participants, the focus is not on the character of an examination, but on the simulation format as training or exercise.
2.2. Evaluation approach
An evaluation was carried out at the end of each simulation. The evaluation questionnaire, which was created using LimeSurvey (version 6.5), includes closed questions (1 “strongly disagree” to 5 “strongly agree”) and open-ended free text questions as well as an overall assessment of the simulation format in the form of a school grade.
The free text fields offer the opportunity to provide information on the following aspects:
- aspects that were particularly liked in the training
- reasons for recommending the training to others
- free feedback option for any further thoughts on the training
- reasons for repeated participation (for those who have participated several times)
In this way, it is possible to find out which aspects are particularly important to the participants because they address these themselves and are not only asked closed questions on predefined aspects. The closed questions on aspects of teaching quality complete the evaluation. Together with the open answers, these can be analyzed using the seven Standford criteria for evaluating clinical teaching [7]. Litzelman et al. [13] have formulated the seven Stanford criteria as shown in table 2 [Tab. 2].
Table 2: Formulation of the Stanford criteria according to Litzelman et al. [13]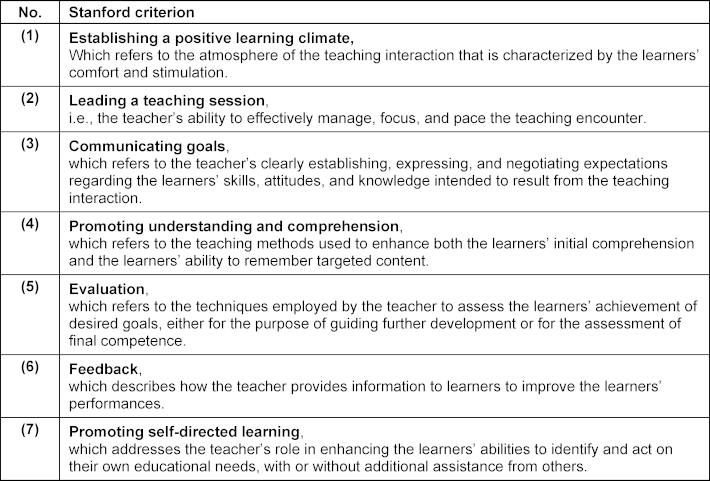
The response rate for the evaluation was 98.7%. A total of 603 participants provided information in the free text fields. The total of 918 free text comments were analyzed using MAXQDA Analytics Pro (version 22.6.0). The comments were assigned to the inductively created categories according to their content. These were in turn assigned to the Stanford criteria of good clinical teaching and then further discussed in order to check the learning objectives. The individual comments generally address several statements, so that some of them were assigned to several content categories, which means that the added percentages in table 3 [Tab. 3] add up to more than 100%. The number per category was set in relation to the total number of free text comments in order to get an impression how relevant which aspects were for the participants.
Table 3: Evaluation results by category and frequency
3. Results
Table 3 [Tab. 3] shows the free texts according to the inductively generated content categories “Quality of the training”, “practical learning content”, “training phases”, “learning atmosphere”, “acknowledgements”, “learning aspects”, “aspects relating to the patients”, “praise of the organization”, and “receiving feedback”. In general, it can be seen that the quality of the training, the practical learning content and aspects of the individual training phases are the most important topics for students when it comes to evaluation. Aspects of the case discussion with an attending are mentioned most frequently (40.5%) when it comes to describing what was liked best. Practicing and learning clinical reasoning and differential diagnostic, a key learning objective of the simulation, is the most common reason why participants would recommend the simulation format to others (43.7%). Aspects of learning and knowledge acquisition and comparison, which are important aspects of self-directed learning, are the most frequently cited reasons for repeated participation (34.6%).
The participants rated the teaching format overall with an average school grade of 1.26±.45. In the following, the evaluation results are structured according to the seven Stanford criteria listed above and examined in more detail:
3.1. Learning atmosphere (criterion 1)
The participants (S1-S23) described a very positive learning atmosphere in the simulation, which apparently led to positive learning outcomes and encouraged repeated participation. A total of 21.1% of the evaluation comments address the positive aspects of the learning atmosphere experienced. The added value lies in this:
Although some of the students report initial fears and concerns about being overwhelmed or similar, in the simulation they experience a “protected environment” (S2) in which they can try things out and achieve learning success:
Participants also praise the pleasant atmosphere, which allows them to make mistakes:
The fun factor is also highly emphasized. This aspect was explicitly mentioned in 69 comments. The combination of fun during clinical work in the simulation with the perception of a challenging course is also evident:
3.2. Leadership (criterion 2)
The participants state that the teachers were able to convey the content of the course well and in a way that was appropriate for the target group (4.70±.51). In the free texts, the good support during the simulation was praised in many cases. Aspects of the evaluation of the didactic concept, which are also frequently mentioned in the comments on what was particularly pleasing, are aspects of general structuring and time structuring, which belong to the Stanford criterion “leadership”. The conceptual planning of the simulation allows it to be effectively managed structurally and the important learning aspects can be perceived in a focused and concentrated manner.
By encouraging and challenging, the teaching staff can adapt the simulation to the learning pace of the students. This is made explicit in the final case discussion, in which the attending physicians’ supervision is described very positively:
The opportunity to work independently is also described very positively:
3.3. Communicating goals (criterion 3)
The participants rated the course as didactically well prepared (4.80±.44) and described the achievement of learning objectives that were implied in the various phases of the simulation:
3.4. Promoting understanding resp. comprehension and self-directed learning (criteria 4 and 7)
In addition to achieving the objectives, the participants clearly describe the successful promotion of understanding and retention of the learning content:
There are also concrete learning experiences that encourage further, self-directed learning:
The perceived sense of responsibility (3.99±.91) is also an important learning experience that can prepare for everyday clinical practice in the initially protected space of the simulation. In addition, the simulation also seems to contribute to leaving one's own “comfort zone” (S17) and gaining self-confidence, which is an important aspect of clinical work for taking up responsibility and working in a team:
As described above, the simulation makes it possible to become aware of one’s own knowledge gaps, learning needs and potential for improvement and thus to support sustainable learning and one’s own control of learning:
Important aspects of self-regulation that arise from self-reflection are revealed and thus activate self-directed learning:
3.5. Evaluation and feedback (criteria 5 und 6)
Self-directed learning was also stimulated by the assessment and feedback in the simulation. The participants received both quantitative assessments as well as verbal and written feedback during and after the simulation. Both the feedback from the teachers (attending physicians) and the feedback from the simulated patients (4.87±.36 and 4.72±.61, respectively) was perceived as very valuable by the participants. Many also emphasized the importance of feedback in their comments. The professional feedback with “good tips” for clinical thinking is very much appreciated and the tips from the simulated patients are seen as helpful for the further development of communication skills.
4. Discussion
The results show a very positive acceptance of the simulation format with clear indications for the implementation of good clinical teaching according to the Stanford criteria and the fulfillment of the learning objectives. The positive perception of the opportunity to work independently is an important learning experience for the participants, especially in view of the fact that this is rarely experienced in this form during their studies and also in the PJ. This also demonstrates the successful integration of the general learning objective of taking responsibility. The space for independence mentioned by the participants, which is perceived as “free” but still functions in the sense of “guided discovery” [14] in the simulation, shows the aspect of successful leadership (criterion 2) and is perceived positively by the participants. In this process of guided discovery, the participants deal with problems (history taking and case preparation) and receive advice (examination findings, support during the case discussion) and feedback (during the case discussion and after the simulation) from the teachers. This approach thus enables students to reflect on their own work process under the guidance of the teacher [15]. This allows the participants to engage in a so-called productive effort, i.e. a challenge in which mistakes can also be made and for which the strongest association with learning success could be shown [16]. A learning atmosphere that is experienced as positive (criterion 1) is an essential component of successful learning [17]. The fun experienced in this not only ensures that the learning environment is perceived positively, but can also contribute to better learning [18], [19]. The learning atmosphere, which is experienced as pleasant and allows mistakes to be made, shows the potential to develop the competence 'dealing with mistakes' in the simulation. The combination of fun, learning challenge and positive learning atmosphere, together with the feedback, create a good balance in the overall learning environment of the simulation, leading to a positive learning experience and the achievement of learning goals in terms of acquiring “adaptive expertise” [12]. Newly acquired motivation and the reports of repeatedly participating persons show that the learning content is sustainably internalized and thus has a consistency that shapes learning, understanding and retention (criterion 4) and that students make sustainable use of the opportunity for self-directed learning (criterion 7).
As participation was voluntary, it cannot be ruled out that particularly motivated students with a positive attitude towards the simulation format took part, which could have had an influence on the evaluation results. In addition, the evaluation was focused on the Stanford criteria, which could have led to other equally important aspects not being sufficiently highlighted. On the other hand, the evaluation data of 868 participants could be analyzed in a standardized way with the help of these Stanford criteria. As required for evaluations [6], various consequences at the structural and procedural level of the simulation format can be derived from the evaluation results. Adjustments to the format were already made during the project as a result of the evaluation findings. For example, an additional training phase has been carried out since 2022, in which students discuss the cases in small groups in advance before case presentation. This corresponds to everyday working life and leads to better achievement of the learning objectives. Further options for adapting the simulation are continuously reviewed on the basis of the evaluation.
5. Conclusion
Based on the standardized evaluation carried out, the integration of the simulation format described here into the curriculum can be recommended. Further development of the format is also possible on this basis. In addition, the simulation format can be used longitudinally and evaluated from this perspective over time.
Notes
Ethics
This project was carried out in accordance with the Declaration of Helsinki. The Ethics Committee of the Hamburg Medical Association approved this project (PV3649). Participation in the formative simulation assessment was voluntary. Written informed consent was obtained.
Funding
This work was supported by the Joachim Herz Stiftung and the Medical Faculty of Hamburg University.
Authors’ ORCIDs
- Sarah Prediger: [0000-0001-5483-1983]
- Sigrid Harendza: [0000-0002-7920-8431]
Acknowledgements
We would like to thank all participants for taking part in the evaluation.
Competing interests
The authors declare that they have no competing interests.
References
[1] Hager P, Gonczi A. What is competence? Med Teach. 1996;18(1):15-18. DOI: 10.3109/01421599609040255[2] Schafer H, van der Blij M, Boon J, van Lieshout H, Schrijen JM. Competentieprofielen: over schillen en knoppen. Fontys. 2002. Zugänglich unter/available from: https://surfsharekit.nl/public/cc2bbd44-4ee4-4199-b6b5-507f4f74009d
[3] Bundesministerium für Gesundheit. Referentenentwurf des Bundesministeriums für Gesundheit. Verordnung zur Neuregelung der ärztlichen Ausbildung. Berlin: Bundesministerium für Gesundheit; 2023. Zugänglich unter/available from: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Gesetze_und_Verordnungen/GuV/A/Referentenentwurf_AEApprO.pdf
[4] Prediger S, Schick K, Fincke F, Fürstenberg S, Oubaid V, Kadmon M, Berberat PO, Harendza S. Validation of a competence-based assessment of medical students’ performance in the physician’s role. BMC Med Educ. 2020;20(1):6. DOI: 10.1186/s12909-019-1919-x
[5] Gibson KA, Boyle P, Black DA, Cunningham M, Grimm MC, McNeil HP. Enhancing evaluation in an undergraduate medical education program. Acad Med. 2008;83(8):787-793. DOI: 10.1097/ACM.0b013e31817eb8ab
[6] Haverkamp N, Barth J, Schmidt D, Dahmen U, Keis O, Raupach T. Position statement of the GMA committee “teaching evaluation”. GMS J Med Educ. 2024;41(2):Doc19. DOI: 10.3205/ZMA001674
[7] Stanford Faculty Development Center for Medical Teachers (SFDC). Core curriculum for clinical teaching seminars. Standford (CA): Standford Faculty Development Center; 2023. Zugänglich unter/available from: https://med.stanford.edu/sfdc/clinical_teaching.html
[8] Harendza S, Gärtner J, Zelesniack E, Prediger S. Evaluation of a telemedicine-based training for final-year medical students including simulated patient consultations, documentation, and case presentation. GMS J Med Educ. 2020;37(7):Doc94. DOI: 10.3205/zma001387
[9] Fürstenberg S, Schick K, Deppermann J, Prediger S, Berberat PO, Kadmon M, Harendza S. Competencies for first year residents - physicians’ views from medical schools with different undergraduate curricula. BMC Med Educ. 2017;17(1):154. DOI: 10.1186/s12909-017-0998-9
[10] Gärtner J, Bußenius L, Schick K, Prediger S, Kadmon M, Berberat PO, Harendza S. Validation of the ComCare index for rater-based assessment of medical communication and interpersonal skills. Patient Educ Couns. 2022;105(4):1004-1008. DOI: 10.1016/j.pec.2021.07.051
[11] Moulaert V, Verwijnen MG, Rikers R, Scherpbier AJ. The effects of deliberate practice in undergraduate medical education. Med Educ. 2004;38(10):1044-1052. DOI: 10.1111/j.1365-2929.2004.01954.x
[12] Clarke SO, Ilgen JS, Regehr G. Fostering adaptive expertise through simulation. Acad Med. 2023;98(9):994-1001. DOI: 10.1097/ACM.0000000000005257
[13] Litzelman DK, Stratos GA, Marriott DJ, Skeff KM. Factorial validation of a widely disseminated educational framework for evaluating clinical teachers. Acad Med. 1998;73(6):688-695. DOI: 10.1097/00001888-199806000-00016
[14] Mayer RE. Should there be a three-strikes rule against pure discovery learning? The case for guided methods of instruction. Am Psychol. 2004;59(1):14-19. DOI: 10.1037/0003-066X.59.1.14
[15] Kua J, Lim WS, Teo W, Edwards RA. A scoping review of adaptive expertise in education. Med Teach. 2021;43(3):347-355. DOI: 10.1080/0142159X.2020.1851020
[16] Kapur M. Examining productive failure, productive success, unproductive failure, and unproductive success in learning. Educ Psychol. 2016;51(2):289-299. DOI: 10.1080/00461520.2016.1155457
[17] Isba R. Creating the learning environment. In: Walsh K, editor. Oxford textbook of medical education. Oxford: Oxford University Press; 2016. p.100-110. DOI: 10.1093/med/9780199652679.003.0009
[18] Gifford H, Varatharaj A. The ELEPHANT criteria in medical education: Can medical education be fun? Med Teach. 2010;32(3):195-197. DOI: 10.3109/01421591003614866
[19] Toufan N, Omid A, Haghani F. The double-edged sword of emotions in medical education: A scoping review. J Educ Health Promot. 2023;12:52. DOI: 10.4103/jehp.jehp_644_21




